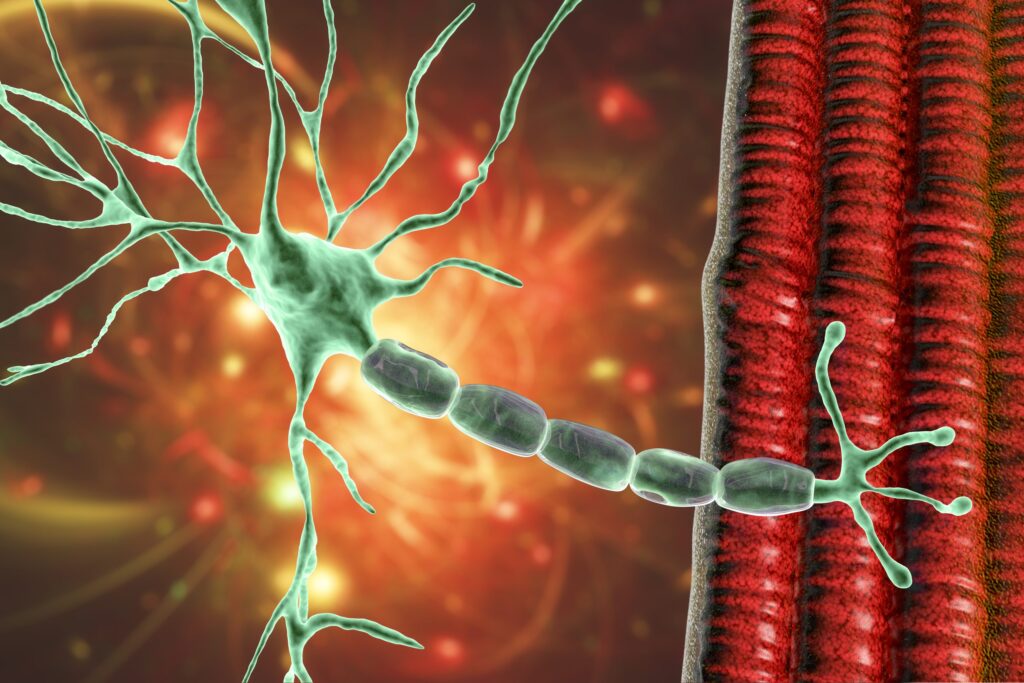
Credit: Dr_Microbe/Getty Images
Amyotrophic lateral sclerosis (ALS) remains one of the most devastating and biologically elusive neurodegenerative diseases. Despite decades of research, its underlying mechanisms are still not fully understood. The condition presents a complex and highly variable interplay of genetic mutations, environmental factors, and cellular dysfunctions that differ widely across patients. This heterogeneity has slowed the development of effective diagnostics and therapeutics, leaving researchers to chase a moving target across a fragmented molecular landscape.
Yet much of ALS research still relies on static models—snapshots of a disease in motion. The condition unfolds dynamically, impacting multiple neural and non-neural cell types in real time. Capturing that progression requires lifelike systems that can replicate ALS as it unfolds in the human body. Without that, critical windows for intervention may remain hidden in plain sight.
In a new study published in Cell Stem Cell titled, “An organ-chip model of sporadic ALS using iPSC-derived spinal cord motor neurons and an integrated blood-brain-like barrier,” researchers at Cedars-Sinai have developed a dynamic ALS model using patient-derived stem cells. This system may help uncover both the causes of ALS and new therapeutic targets.
The approach builds on earlier research in which ALS patient cells were reprogrammed into induced pluripotent stem cells (iPSCs) and then differentiated into motor neurons, the very cells that degenerate in ALS, leading to the progressive loss of movement, speech, and ultimately, the ability to breathe.
To create the organ-chip ALS model, the researchers seeded iPSC-derived spinal cord motor neurons from ALS patients into the top channels of a microengineered chip. Cells that form the blood-brain barrier were seeded into the bottom channels. The two compartments were connected by a porous membrane, enabling the flow of fluid to simulate blood circulation.
A control set of chips was also generated using cells from individuals without ALS. Using advanced transcriptomic tools, the team analyzed more than 10,000 genes in the motor neurons of both groups. The team also used proteomics and single nuclei RNA sequencing to identify distinct motor neuron subpopulations with ALS-specific dysregulation in neurofilaments, glutamatergic, and synaptic signaling.
“In our early work, we couldn’t detect many differences between the motor neurons of patients with ALS and those from healthy individuals,” said Clive Svendsen, PhD, executive director of the Board of Governors Regenerative Medicine Institute at Cedars-Sinai and senior author of the study. “But those studies employed traditional lab culture that is static, like a pond. In the body, blood vessels provide constant fluid flow to bring in nutrients and take away waste, and may even provide other types of support to motor neurons.”
Motor neurons matured more completely in the chip-based system compared to static culture dishes. The researchers observed distinct gene expression differences in ALS patient-derived cells, particularly in glutamate signaling pathways.
“We were intrigued to find that signaling for glutamate, a chemical that sends excitatory messages between neurons, was altered in the ALS motor neurons,” Svendsen said. “Excessive release of glutamate has long been considered a possible cause of ALS, and one of the few drugs approved to treat the disease targets this neurotransmitter. The changes we found don’t seem to cause any issues for the motor neurons when they are young, but over many years, it is possible that this increased glutamate signaling may be part of why motor neurons die in ALS.”
The researchers now aim to determine whether this altered signaling directly causes motor neuron dysfunction or death. While glutamate may be just one piece of the puzzle, the team noted that their model potentially offers a powerful tool to investigate additional mechanisms.
“We haven’t connected all the dots yet,” said Svendsen, “but based on these findings, we have a model that will allow us to test our theories. If we can show that glutamate signaling eventually makes the ALS motor neurons sick, for instance, we can apply drugs to the blood vessel side of the chip to mimic a clinical trial. Those experiments are underway.”