A groundbreaking advancement in dermatological diagnostics has emerged from a multidisciplinary research collaboration at Kindai University Faculty of Medicine and the Faculty of Engineering. This team, spearheaded by Drs. Haruyo Yamamoto, Chisa Nakashima, and Atsushi Otsuka, has succeeded in developing a highly accurate artificial intelligence (AI)-driven classification system dedicated to the identification and categorization of facial pigmented lesions. These lesions, which pose significant diagnostic challenges due to their visual similarity, are crucial to distinguish accurately as they have direct implications on treatment modalities, particularly laser therapies. This pioneering work was detailed in a recent publication in the international medical journal Cureus on June 5, 2025, marking a notable leap forward in medical AI applications for dermatology.
Facial pigmented lesions encompass a broad spectrum of dermatological conditions, including melasma, ephelides (commonly known as freckles), acquired dermal melanocytosis, solar lentigo, and lentigo maligna melanoma (LM/LMM). Despite their varied etiologies and prognoses, these lesions often present with overlapping morphological features that confound even experienced dermatologists. Traditional diagnostic reliance on visual examination and histopathological confirmation faces limitations due to subjective interpretation and the invasiveness of biopsies. The efficiency and accuracy in classifying these lesions are paramount, given that misdiagnosis can lead to inappropriate treatment strategies—such as the exacerbation of melasma through misguided laser intervention or the dangerous delay in surgical excision for malignant lesions like LM/LMM.
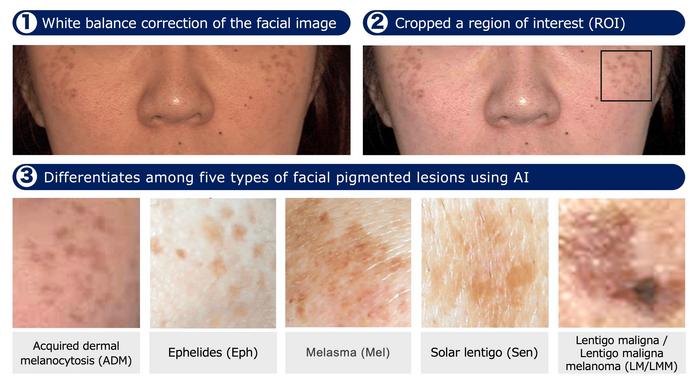
Leveraging the power of deep learning, the research team engineered a dual-model system utilizing InceptionResNetV2 and DenseNet121 architectures—both renowned for their high performance in image classification tasks. These convolutional neural networks (CNNs) were trained on a robust dataset of 432 clinical images, meticulously preprocessed through established computer vision pipelines. Central to this preprocessing was the correction of white balance using OpenCV’s Python library to standardize color representation, ensuring that skin tone variations did not bias the model’s learning. Subsequently, a square region of interest (ROI) encapsulating the primary lesion area was extracted to focus the neural networks’ attention on relevant features, excluding extraneous skin or background elements. Only images with sufficient clarity, as determined by a Laplacian variance threshold of 10, were included to guarantee data quality and model reliability.
.adsslot_qxYm9C7zHT{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_qxYm9C7zHT{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_qxYm9C7zHT{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The system’s diagnostic performance was rigorously compared against the expertise of 20 dermatologists, differentiated into board-certified specialists and non-certified practitioners. Impressively, both InceptionResNetV2 and DenseNet121 achieved diagnostic accuracies of 87% and 86%, respectively, significantly outperforming the median accuracy of expert dermatologists at 80% and markedly exceeding the 63% median accuracy displayed by non-experts. This breakthrough is particularly striking in the system’s capacity to detect LM/LMM, where both models demonstrated perfect sensitivity (100%). Accurately identifying this malignant entity bears significant clinical importance, reflecting the system’s potential as a life-saving diagnostic adjunct.
Deep learning’s success in medical image analysis has notably transformed fields such as melanoma detection, yet its application to a broader range of pigmented facial lesions had remained underdeveloped until now. This research closes a critical gap by addressing lesions that are subtle yet consequential for laser treatment decisions. The automated classification system stands to reduce diagnostic errors and the associated risks of mistreatment, thus delivering tangible benefits in both healthcare quality and patient safety. Moreover, by furnishing dermatologists with precise lesion classification, the AI system can streamline clinical workflows and enhance decision-making efficiency.
The researchers emphasize not merely the accuracy of their models but also the clinical utility regarding treatment guidance. Given the nuanced treatment algorithms applicable to each lesion type, the AI’s ability to delineate lesion classes supports tailored therapeutic interventions. For example, despite the superficial similarities between solar lentigo and melasma, their pathophysiologies and responses to laser treatment differ significantly. The AI system’s reliable categorization ensures that patients receive the most appropriate laser protocols, minimizing adverse effects and maximizing therapeutic efficacy.
A sophisticated preprocessing pipeline differentiates this framework from traditional image classification efforts. Through correcting color imbalances, isolating lesions, and filtering for image clarity, the model circumvents common pitfalls related to skin tone heterogeneity and image artifacts. This attention to preprocessing detail enhances the deep learning models’ generalization capabilities—a crucial aspect for deployment in real-world clinical settings marked by variable image acquisition conditions.
Training and validation steps involved comprehensive cross-validation processes to mitigate overfitting and ensure consistent performance across diverse cases. The involvement of both expert and non-expert dermatologists as comparators adds a rigorous benchmark for evaluating clinical relevance. The AI models not only matched but in many areas surpassed human diagnostic abilities, underscoring the transformative potential of integrating AI tools into dermatology practice.
The implications of this research extend beyond diagnostic accuracy; it signals a paradigm shift wherein AI can function as a co-pilot to dermatologists. Rather than replacing clinical judgment, the technology amplifies it, enabling more nuanced and confident decision-making. This collaborative dynamic holds promise for democratizing access to high-quality dermatological care, especially in regions lacking specialist availability.
Future directions envisaged by the authors involve expanding the dataset to include more diverse skin types and lesion variants, thereby improving the robustness and inclusivity of the AI system. Additionally, integrating this diagnostic tool into portable imaging devices could facilitate point-of-care assessments, broadening the scope for teledermatology and remote clinical consultations. Such advancements could herald an era of democratized healthcare, where accurate skin lesion diagnosis is accessible globally through AI-enhanced technologies.
This study exemplifies the power of interdisciplinary collaboration, melding clinical insights with cutting-edge engineering techniques to address a persistent challenge in dermatology. The authors’ transparent methodology, including available digital object identifiers (DOI) and open access publication in Cureus, invites replication and further innovation. As the medical community continues to embrace AI, such pioneering efforts pave the way for safer, more precise, and personalized dermatological care.
In sum, the AI-based classification system developed by Kindai University researchers represents a significant step forward in the accurate diagnosis of facial pigmented lesions. Achieving performance metrics that surpass human experts, it promises to radically improve treatment decision-making, particularly for complex conditions requiring laser therapy. This integration of deep learning into clinical workflows stands to not only enhance patient outcomes but also to reshape how dermatological expertise is delivered worldwide.
Subject of Research: People
Article Title: Deep Learning-Based Classification System for Facial Pigmented Lesions to Aid Laser Treatment Decisions
News Publication Date: 5-Jun-2025
Web References: DOI: 10.7759/cureus.85428
Image Credits: Professor Atsushi Otsuka, Kindai University Faculty of Medicine, Japan
Keywords: Melanoma, Deep learning
Tags: accurate classification of skin lesionsadvanced artificial intelligence in medicineAI-driven dermatology diagnosticschallenges in diagnosing facial lesionsCureus journal publication on AI in healthcaredermatology research collaborationfacial pigmented lesions classificationimproving accuracy in dermatological treatmentslaser therapy implications in diagnosismelasma and skin condition identificationmultidisciplinary approach in medical researchnon-invasive diagnostic techniques in dermatology