Immuno-oncology seeks to harness the body’s immune system to identify and destroy cancer cells. Although often considered a modern medical breakthrough, its roots trace back to the late 19th century. During this time, William Bradley Coley, MD at the New York Hospital (now the Weill Cornell Medical Center) made the fascinating observation that several cancer patients had experienced spontaneous remission after contracting streptococcal infections. Coley believed the immune response drove the remissions, and he undertook the injection of bacteria into tumors as a potential treatment for bone cancer. Over a century after this early foray into immuno-oncology, the field is rapidly advancing with checkpoint inhibitor drugs, CAR T-cell therapies, and innovative cancer vaccines. GEN spoke with four leading companies to highlight how the latest breakthroughs are shaping the present and future of this longstanding field.
Employing pairs of cytokines
Deka Biosciences is developing new therapeutic modalities called DiakinesTM that consist of paired cytokines, natural proteins that can stimulate or suppress the immune system. John B. Mumm, PhD, Deka’s president and CEO, explains that cytokines are natural proteins that variously affect the immune system.

President and CEO
Deka Biosciences
“There are stimulatory cytokines that activate the immune system and inhibitory cytokines that shut down things like inflammation,” Mumm says. “If you really want to push biology in a therapeutically relevant direction with cytokines, you need more than one.”
Deka Biosciences’ leading immuno-oncology platform combines interleukin 2 (IL-2) with interleukin 10 (IL-10). Mumm explains that the IL-2 stimulates the immune system to fight cancer, while the IL-10 minimizes toxicity. “IL-2 is like jet fuel. It massively activates the immune system, but it is super toxic. Meanwhile, IL-10 is one of nature’s anti-inflammatories. The presence of IL-10 compresses that fuel into a useful direction, like the nozzle of a jet engine.”
Mumm explains that these paired cytokines accumulate in tumors by binding to the EGF receptor on the surfaces of the tumor cells. “This keeps the T cells stuck to the tumor cells and further enhances the potency,” he says.
In its Phase I study, the company has treated 35 patients with EGF receptor-positive tumors who have experienced relapses on checkpoint inhibitors. “Our studies indicate that our Diakines are super-safe,” says Mumm. “Because of the IL-10, we block cytokine release syndrome and avoid common IL-2 side effects like vascular leaks.”
Mumm also notes that around 50% of patients have exhibited radiologically stable disease at the first scan. Furthermore, he says that he expects to see partial responses once patients are on treatment longer.

Diakines are available as a convenient off-the-shelf therapy that can be dosed at home. Furthermore, the platform has a personalized component. “Our tagline mission is that we can build a Diakine for every patient,” says Mumm. “We are building assay systems and understanding the genetics behind who is likely to respond to a given cytokine pair.”
Finally, Mumm is optimistic about combining Diakines with other treatments. He notes that IL-2 is often administered along with CAR T-cell therapy and cancer vaccines. “Now that we have solved the problem of IL-2 toxicity, Diakines can be combined with these therapies to reduce toxicity and dramatically enhance function,” he says.
Anchoring drugs to the tumor site
Howard L. Kaufman, MD, president and chief executive officer of Ankyra Therapeutics, explains that ankyra is the Greek word for anchor. “Our company is all about anchoring. We are trying to anchor or retain drugs in the tumor microenvironment.”
Kaufman explains that Ankyra has developed aluminum hydroxide as a scaffold to which toxic cytokines like interleukin 12 can be attached. “Aluminum hydroxide is a really interesting compound,” Kaufman says. “It is an inert metal that tends to stay where you put it. We directly inject it into the tumor, and our modeling predicts that it may be retained for up to 12 weeks.”

President and CEO
Ankyra Therapeutics
Kaufman compares Ankyra’s technology to antibody-drug conjugates, which use antibodies to bind to specific tumor-site antigens to deliver toxic drug payloads. However, he notes that cancer cells often down-regulate these antigens over time, diminishing the effects of treatment. “The advantage of our drug is that it will sit there much longer because it is anchored to the aluminum hydroxide,” he says.
Kaufman highlights the company’s Phase I study in dogs with melanoma. “We treated 18 dogs with a canine version of our drug,” he says. “There were no major safety signals, and some of these dogs are still alive two years after treatment without evidence of disease.”
Ankyra has also begun a Phase I study in people with accessible lesions like skin cancer. “We have tested the drug at six different doses, and, to date, we see no dose-limiting toxicities in any of the patients.”
The Phase I study is also showing signs of biological activity. “Many patients with one dose of our drug experience a ten-fold increase in T cells coming to the tumor site,” according to Kaufman. “In gene expression profiles, we also see significant upregulation of several pro-inflammatory genes involved in activating the immune system.”

In the future, Ankyra hopes to add monoclonal antibodies to its scaffolds. It has also started a Phase I study to inject its treatment directly into solid tumors in the lungs, liver, and other visceral locations.
Making CAR T cells more accessible
Steve Harr, MD, president and chief executive officer of Sana Biotechnology, is optimistic about CAR T-cell therapy, noting that “In many settings, it produces durable and complete responses that may be curative in one-third to one-half the blood cancer patients who receive them.”

President and CEO
Sana Biotechnology
However, Harr also notes that most people who would benefit from CAR T-cell therapy—including those in the United States—will die without receiving it. “Most patients cannot access those drugs globally because they take time to manufacture, manufacturing capacity is limited, they are expensive, and hospital capacity is limited,” he says.
Although multiple CAR T-cell therapies have been approved, Harr notes that all of them are autologous, meaning that the patient’s own cells are genetically reprogrammed in a time-consuming and expensive process. In contrast, Sana is taking a different approach—referred to as allogeneic CAR T-cell therapy—in which donor T cells are reprogrammed in a manufacturing process that creates enough medicine to treat hundreds of patients.
“Unlike autologous CAR T-cell therapy, our technology is scalable and cheaper to make. The technology offers the potential for patients to have off-the-shelf therapy to treat their cancer immediately when it is needed,” says Harr, who also stresses that the company’s key challenge has been to overcome allogeneic recognition and rejection. “If somebody put my cells into you, your immune system will recognize them as foreign and kill them,” Harr notes. He explains that Sana’s hypoimmmune technology resolves this problem by genetically reprogramming the cells so that a recipient’s body will not recognize them as foreign.
But how do we know that allogeneic CAR T-cell therapy is safe? “We have to approach biology with a lot of humility,” stresses Harr. “It is incumbent on us to take our time through dose escalation to ensure we do the right thing for patients.”
Nevertheless, Harr emphasizes that data from the company’s dose escalation study in leukemia and lymphoma showed “a good safety profile and early evidence that the patient’s immune system does not recognize these allogeneic cells.” Furthermore, two out of four patients experienced complete responses, meaning they had no detectable cancer. “I think we have reasons to be encouraged,” concludes Harr.
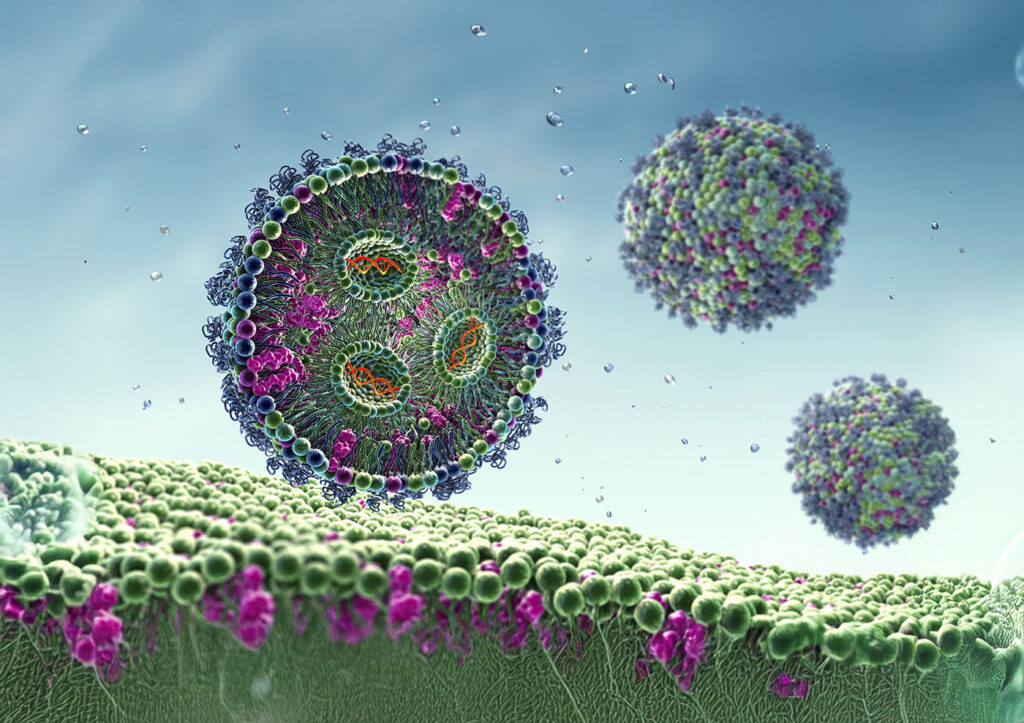
Lipid nanoparticles deliver mRNA to fight cancer
Lipid nanoparticles—called LNPs—are tiny, spherical lipid particles used to deliver various cargoes, such as mRNA, for vaccines or genomic medicines. Kate Zhang, PhD, chief scientific officer of Hopewell Therapeutics, notes that LNPs provided the mode of delivery for the Pfizer-BioNTech and Moderna COVID-19 vaccines. “However, even though LNP technology has demonstrated its overall safety through the broad use of COVID vaccines,” Zhang says, “we still need to demonstrate its safety for other therapeutic applications.”

Chief Scientific Officer
Hopewell Therapeutics
Zhang further explains how Hopewell is using tissue-targeting LNPs encapsulating mRNA-encoded therapeutic proteins to treat various diseases. “We can optimize the lipid structure and formulation of these LNPs to target specific organs with specific cargo types,” she notes.
In the realm of immuno-oncology, the company is currently developing LNPs to deliver mRNA-encoding bispecific T-cell engagers (BiTEs) to treat both hematologic malignancies and solid tumors. Zhang explains that BiTEs are single-chain proteins with two different antigen-binding sites that can recruit cytotoxic T cells to cancer cells, destroying the tumor cell.
Hopewell’s strategy has many advantages over conventional recombinant BiTEs, which are typically administered intravenously and often result in serious adverse events like cytokine release syndrome and neurotoxicity. In contrast, Hopewell’s LNP-based approach allows for the direct delivery of the therapeutic agent to the organs of interest, minimizing side effects from whole-body exposure.
Hopewell’s lead development program encodes a specific type of BiTE (a CD19-CD3 T-cell engager) to treat B-cell malignancies. “This LNP targets the liver, lymph nodes, and bone marrow so that B cells can be targeted,” she explains.
Zhang highlights that the company’s multiple BiTE assets have achieved preclinical proof of concept. Meanwhile, its lead BiTE asset has demonstrated favorable properties in nonhuman primates. “Our goal is to initiate IND-enabling studies and hopefully bring the drug candidate to clinical development soon,” she says.
The future of immuno-oncology
What does the future of immuno-oncology hold? Will it be dominated by cytokine-based therapies, gene therapies, CAR T-cell treatments, or some other emerging approach? “I think all of the above,” says Harr. “Cancer is a complicated adversary. We would be crazy to ignore any of these tools in our toolbox.”