Voltage-gated sodium channels (VGSCs) are integral membrane proteins essential for the generation and propagation of action potentials in excitable cells. Among them, NaV1.2 is particularly noteworthy due to its pivotal role in neuronal signaling. Understanding its structure and function has profound implications not only for neuroscience but also for addressing a vast array of pathologies linked to sodium channel dysfunctions. A recent study by Oliveira-Madureira, Leal, and Azevedo takes an innovative approach by investigating the structural perspectives of genetic variability associated with NaV1.2, unveiling layers of complexity previously overlooked.
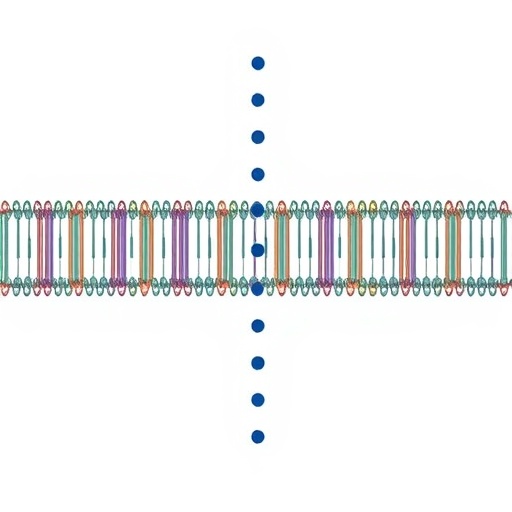
At the heart of NaV1.2’s function is its unique structural configuration. The channel comprises four homologous domains, each contributing to the channel’s ability to facilitate sodium ion conduction across the plasma membrane. The arrangement allows NaV1.2 to respond effectively to physiological stimuli, such as membrane depolarization. The researchers emphasize that even slight alterations in its structure can lead to significant functional consequences, a revelation that enhances our understanding of how genetic variations can impact neural activity and overall brain function.
The genetic variability surrounding NaV1.2 is particularly interesting, especially in the context of neurological disorders. The study highlights several mutations and polymorphisms that can alter channel biophysics, leading to conditions such as epilepsy, cardiac arrhythmias, and other sodium channel-related diseases. Each genetic variant brings its distinct challenges, necessitating a deeper investigation into how these variations affect channel behavior from a molecular standpoint.
To elucidate these genetic influences, the authors meticulously discuss advanced techniques employed in protein structural analysis. High-resolution X-ray crystallography and cryo-electron microscopy are pivotal methods that offer insights into NaV1.2’s complex architecture. These techniques allow researchers to visualize conformational changes in response to voltage fluctuations, improving our grasp on how the channel achieves its functional state. This structural insight is complemented by computational modeling, which predicts how various genetic variants might alter the channel’s dynamics.
Another significant aspect of the study involves the role of post-translational modifications (PTMs) in regulating NaV1.2 activity. The researchers review evidence suggesting that phosphorylation, glycosylation, and other PTMs can significantly modulate channel properties. Such modifications represent an additional layer of variability that can be influenced by genetic factors, further complicating the relationship between genotype and phenotype. In their analysis, Oliveira-Madureira et al. emphasize that understanding these PTMs may provide therapeutic avenues for conditions precipitated by dysregulated sodium channel activity.
In their concluding sections, the authors turn their attention to the implications of their findings for future research and therapeutic strategies. The structural insights gained from their investigations are poised to inform drug development processes aimed at targeting NaV1.2 specifically. For instance, drugs designed to enhance or inhibit channel activity could mitigate the effects of detrimental mutations, thereby restoring normal physiological function. This bodes well for developing personalized medicine approaches, where treatment strategies could be tailored based on individual genetic profiles.
Moreover, the interplay between sodium channel architecture and pharmacology is discussed in detail. The authors mention recent breakthroughs in understanding how traditional anti-epileptic drugs (AEDs) interact with NaV1.2, highlighting the potential to refine existing therapies and create novel agents that more effectively target specific genetic variants. This aspect is critical for advancing treatments that rely on the precision modulation of ion channel functions.
The study then shifts to a discussion on the broader implications of VGSC research. Voltage-gated sodium channels are present in virtually all excitable tissues — not just the nervous system, but also in cardiac and skeletal muscle cells. The understanding gained from NaV1.2 could thus have far-reaching consequences for comprehending various physiological processes and diseases beyond neurobiology, extending into cardiovascular health and muscle disorders.
As the conversation around sodium channels evolves, so does the necessity for interdisciplinary approaches that bridge genetics, molecular biology, and pharmacology. The contribution from Oliveira-Madureira and colleagues emphasizes that collaborative research efforts will be vital for unraveling the complexities of NaV1.2 and similar channels in the context of human health. Pipelines that integrate structural, genetic, and clinical data offer the best chance for transformative breakthroughs in both understanding and treating related pathologies.
Looking forward, the need for robust databases capturing genetic variations associated with VGSCs is underscored. Such resources would enable researchers to correlate specific genetic polymorphisms with functional outcomes more efficiently. This could streamline the process of identifying at-risk individuals and informing treatment decisions based on robust genetic evidence.
As one of the most studied ion channels, NaV1.2 serves as a fundamental model for understanding VGSCs. The ongoing research endeavors in this domain not only deepen our understanding of basic neural function but also present the groundwork for novel therapeutic strategies aimed at a range of conditions influenced by sodium channel dysfunction. The future of sodium channel research appears bright, fueled by continuous technological advancements and a critical focus on genetic variability — factors that are likely to characterize the next generation of neuroscience research.
In summary, this insightful study elevates the discourse surrounding voltage-gated sodium channels, particularly highlighting NaV1.2 as a critical player in both health and disease. The elucidation of structural variations and their functional consequences paves the way for innovative therapeutic approaches and reinforces the importance of genetic consideration in biomedical research. With these findings, Oliveira-Madureira, Leal, and Azevedo have not only contributed to the scientific community’s understanding of NaV1.2 but have also set the stage for future research endeavors that may lead to significant medical advances.
Subject of Research: Voltage-Gated Sodium Channel NaV1.2
Article Title: Voltage-Gated Sodium Channel NaV1.2: Structural Perspective of the Genetic Variability.
Article References:
Oliveira-Madureira, T., Leal, B. & Azevedo, L. Voltage-Gated Sodium Channel NaV1.2: Structural Perspective of the Genetic Variability.
Biochem Genet (2026). https://doi.org/10.1007/s10528-026-11327-z
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s10528-026-11327-z
Keywords: Voltage-gated sodium channels, genetic variability, NaV1.2, structure-function relationship, neurological disorders, pharmacology, post-translational modifications, personalized medicine.
Tags: biophysics of NaV1.2 mutationseffects of structural changes on channel functiongenetic variability of sodium channelsimplications of sodium channel mutationsinnovative research in neuroscienceNaV1.2 channel structure and functionneurological disorders related to sodium channelsneuronal signaling and action potentialsneuroscience and genetic researchpathologies linked to NaV1.2sodium ion conduction mechanismsvoltage-gated sodium channel dysfunction