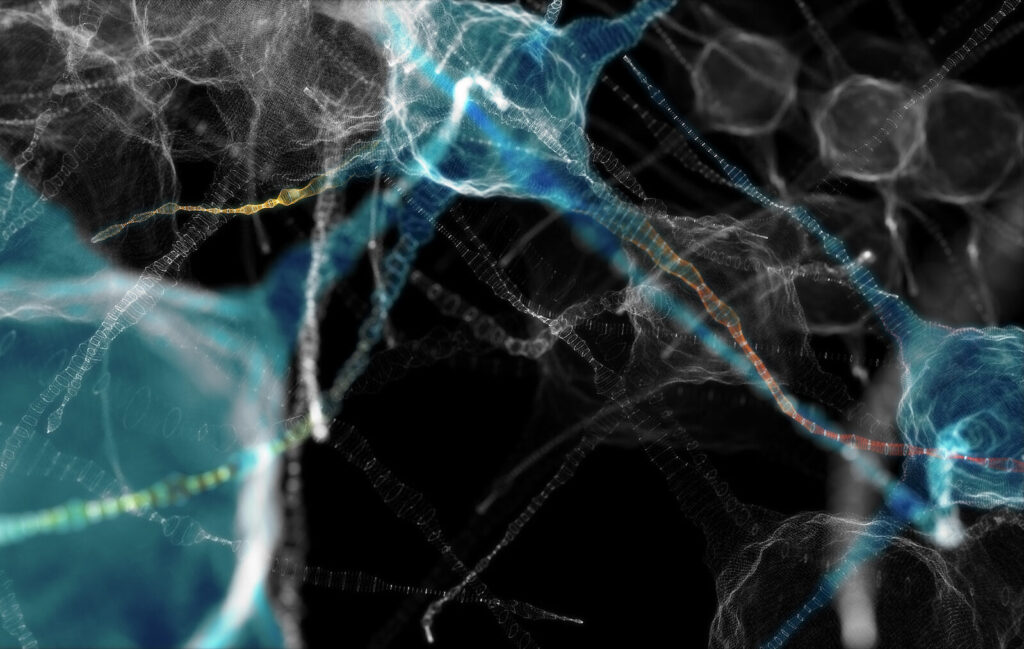
As people age, their risk of developing neurodegenerative disorders like dementia, Alzheimer’s disease, and Parkinson’s disease increases. A new study from scientists at the University of California, San Diego (UCSD), helps elucidate some of the molecular mechanisms behind why brain cells deteriorate with age. Specifically, they found that old neurons have dysregulated RNA metabolism that dampens their stress response and makes them susceptible to neurodegeneration.
Details of the study are published in a Nature Neuroscience paper titled, “Neuronal aging causes mislocalization of splicing proteins and unchecked cellular stress.” The team was led by Gene Yeo, PhD, a professor in the department of cellular and molecular medicine at UCSD, and director of the university’s Center for RNA Technologies and Therapeutics. According to the paper, they found evidence that aged neurons “are broadly depleted of RNA-binding proteins, especially spliceosome components.” They also found links between chronic stress and malfunctioning ubiquitylation machinery as well as poor chaperon protein activity and the inability of older cells to respond to new sources of stress.
“Aging has been a black box for a long time,” Yeo said. Currently, “nobody is really sure what an aged neuron looks like, how it behaves, or how it’s different from a young neuron.” To attempt to answer that question, he and his team generated aged neurons by reprogramming skin cells from aged healthy human donors, bypassing the pluripotent stem cell state. They then compared the old neurons to young neurons.
Their comparison revealed that older neurons had various hallmarks of molecular stress such as storing untranslated RNA and protein in stress granules—compartments outside of the cell’s nucleus. They found evidence of the “depletion of the chaperone HSP90α from stress granules” which “regulates the ubiquitinome” and is “required for proper resolution of stress granules.”
Aged neurons also took much longer to recover from acute stress than young neurons and failed to make stress-responsive proteins, according to the findings. Furthermore, the scientists observed issues with splicing proteins like TDP-43 protein, which regulates gene expression in young neurons. Specifically, these proteins accumulate and “mislocalize to the cytoplasm in aged neurons, which leads to widespread alternative splicing,” the scientists wrote. Neurons in patients with Alzhiemer’s, dementia and other disorders exhibit similar behavior. In fact, “TDP-43 forms cytoplasmic aggregates in >95% of patients with ALS,” the researchers noted in the paper. TDP-43 aggregation is also implicated in over 50% of Alzheimer’s cases.
The findings suggest that “aged neurons are prioritizing other proteins and forgetting about the stress response and about RNA-binding proteins that keep everything running smoothly,” Yeo said. While more data is needed, it is possible that “reversing chronic stress may be a viable therapeutic avenue to prevent neurodegeneration and should be a focus of future efforts to promote the healthy aging of neurons,” the scientists wrote.