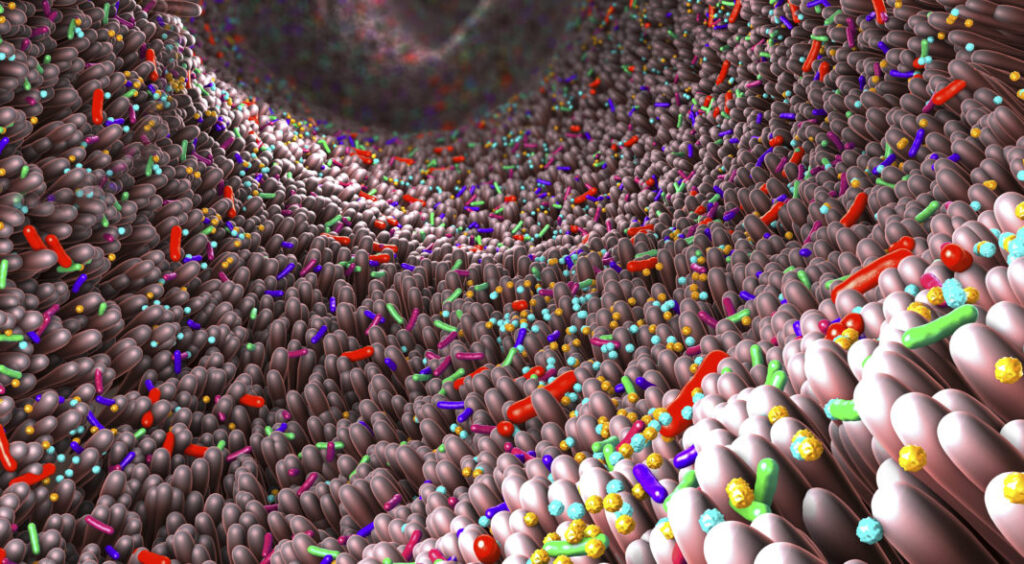
Credit: Christoph Burgstedt/Science Photo Library
Fecal microbiota transplants (FMT) have been touted as a potential treatment for a variety of conditions, from inflammatory bowel diseases (IBDs), obesity, and type 2 diabetes, to autism. The results of new research carried out by researchers at the University of Chicago, now caution against widespread use of FMT because of the potential for long-lasting, unintended health consequences for recipients.
In experiments with mice and studies with human tissue samples, the researchers saw that anaerobic microbes from the colon not only colonized the small bowel after a single transplant but also persisted there for months. These microbes also changed their new intestinal environments to their advantage, “terraforming” them in ways that caused changes in the recipient’s metabolism, behavior, and energy balance.
“I think it’s a bit of a wakeup call to the field that maybe we shouldn’t willy-nilly put large bowel microbes into different parts of the intestine that shouldn’t be there,” said Orlando (Landon) DeLeon, PhD, a postdoctoral researcher at UChicago and lead author of the new study, which was published in Cell. “If we’re designing good therapeutics, we should be aware of the importance of matching the regional microbiota to their proper environments, so that we provide better overall health benefits.” The investigators’ published paper is titled “Microbiome mismatches from microbiota transplants lead to persistent off-target metabolic and immunomodulatory effects,” in which they concluded, “… regional microbial mismatches after FMTs can lead to unintended consequences and require rethinking of microbiome-based interventions.”
FMT involves transferring microbes in the stool from a healthy person to a sick one, in hopes of restoring a healthy equilibrium in the gut microbiome. Fecal microbiota transplant (FMT) is an increasingly used intervention to promote repair of intestinal dysbiosis,” the team wrote. FMT is approved by FDA only for treating repeated infections with Clostridium difficile (C. diff), an opportunistic bacterium that often causes severe gastrointestinal symptoms and inflammation in hospital patients who have been on antibiotics. Seeing the success in treating C. diff patients, many physicians have been eager to use FMT to treat other digestive conditions.
Researchers understand that gut microbiome health can impact all vital organs and systems of the body, so the idea is that replacing a “sick” gut microbiome with a “healthy” one could fix the problem in one fell swoop. But, as the authors pointed out, “Although FMT is effective for recurrent Clostridioides difficile infection, its mechanisms, efficacy, and off-target consequences in other disorders, including obesity, autism, cancer, and inflammatory bowel diseases, remain unclear.”
The gut isn’t simply one consistent environment with the same microbiota throughout. Instead, it has several distinct regions that are vastly different microbial ecosystems, each tailored for specific microbes that can provide functions vital to the health of their host.
Since stools contain primarily anaerobic microbes from the colon, FMT can cause mismatches in the gut ecosystem when those bacteria colonize the small intestine and other parts of the digestive system. The authors suggest that the suitability of FMT as an intervention to restore regional gut microbiota, particularly in the small bowel (SB), “… must be questioned because of its predominant anaerobic composition.”
They noted, “Considering that large bowel microbiota (LBM) are predominantly anaerobic and differ in composition and function to SBM, the appropriateness of FMT to reconstitute the SB must be questioned as they are composed of non-indigenous and likely unfit microbes.” DeLeon added, “There are microbes along the entire intestinal tract, and we just study predominately the last third of it (the colon). So, how can you expect an FMT, with microbes from a third of the intestinal tract at the end of it, to fix the rest of the intestine?”
To test the effects of FMT on different parts of the intestine, DeLeon, together with colleagues including senior author Eugene B. Chang, MD, the Martin Boyer Professor of Medicine at UChicago, carried out a series of experiments with mice. Recipients of FMT are usually treated with antibiotics first to clear out the microbes living in the gut, leaving a clean slate for newly transplanted microbes to take up residence. For their reported study, one group of animals was given a transplant of microbes taken from the jejunum, which is the first portion of the small intestine. A second group was given a standard FMT, and a third group was given a transplant from the cecum, a section connecting the small and large intestine, which has a mixture of microbes from both. “… antibiotic-treated specific-pathogen-free (SPF) mice were given jejunal, cecal, or fecal MTs (JMTs, CMTs, or FMTs, respectively) and studied 1 or 3 months later,” the team wrote in summary.
Their findings showed that microbes from each of these transplants successfully colonized the entirety of the intestinal tract in the mice, not just their native niches. This created regional gut mismatches persisting up to three months after just one transplant. The results, they reported “demonstrate that a single MT of SBM and LBM can successfully engraft the entirety of the intestinal tract (not only their native niche), that it can change the regional microbial composition and functional potential, and that this colonization is persistent. This extends the parallel observations of increased and persistent anaerobic colonization of the SB after FMT in humans.”
The altered microbiomes also changed the production of metabolites in each intestinal region, which can have health effects on the host. The researchers saw changes in liver metabolism, including activity in genes associated with immune function. “It is clear that transplantation of native vs. non-native microbes yield drastic changes in microbiota composition and function to affect host metabolism and distal organs (i.e., the liver),” they stated. The investigators also observed differences in eating behaviors, activity, and energy expenditure in the mice after transplants.
The most striking finding was that having the wrong microbes in the wrong place reshaped the tissue identity to make it more suitable for them. The researchers observed that mismatches changed gene and protein expression in the intestinal lining in ways that more closely resembled expression levels from the microbes’ original or native intestinal regions. “It’s like they’re engineering or terraforming their environments to help them fit in,” DeLeon said. The authors stated that their data, “… suggest that mismatched, non-native microbes can re-program the identity of the tissue, enhancing genes conducive to adaptation and engraftment.”
The results of tests on human tissues corroborated the team’s murine results, “… supporting the finding that microbes are able to shift mucosal ecosystems to fit their native environment’s signature and that these processes can occur in humans.” Chang said that the research highlights the need for more caution with FMT before we fully understand the long-term effects of introducing one set of microbes into a new environment. “We have absolutely no idea what’s in FMT, except that it’s a combination of microbes,” Chang said. “But even a single FMT will cause a change in the host-microbe relationships in these very different regions of the bowel that may be very difficult to reverse.”
In their paper the team noted, “These data raise a cautionary note, that unrecognized short and long-term consequences of the FMT may emerge in clinical practice, in particular for off-label use where mechanism and efficacy remain unknown…At the very least, these data demonstrate that fecal microbiota that normally comprise FMTs are not sufficient to reconstitute the entire gut and can cause undesired, off-target effects.”
Both DeLeon and Chang advocate for “omni-microbial transplants,” or OMT, instead. This approach would transfer microbes taken from all the different regions of the intestine, not just those largely from the colon. Whether given via an endoscopy or in pill form, microbes naturally settle in the right places, especially when they are competing side by side with others that normally inhabit a certain region. “If there’s an open space, something’s going to fill it,” DeLeon said. “But the microbes that were supposed to be there are better suited for it, so they’re more naturally going to fill it even in the presence of other microbes.”
DeLeon plans to keep studying how different microbes exert their influence in different parts of the intestine, using different approaches like single cell sequencing and metabolomics to track their activity. He is also exploring how the gut regions terraformed by microbiota mismatches can be restored to their original state, which could help restore normal gut function. Such deeper understanding could lead to improvements in the application of microbial transplants, ultimately helping them live up to their significant promise.
The authors also concluded, “Future studies will also focus on determining the long-term implications of FMT on host metabolism and immune function, such as after six months to one year post transplant, and the effects on other organ systems, including the brain.”