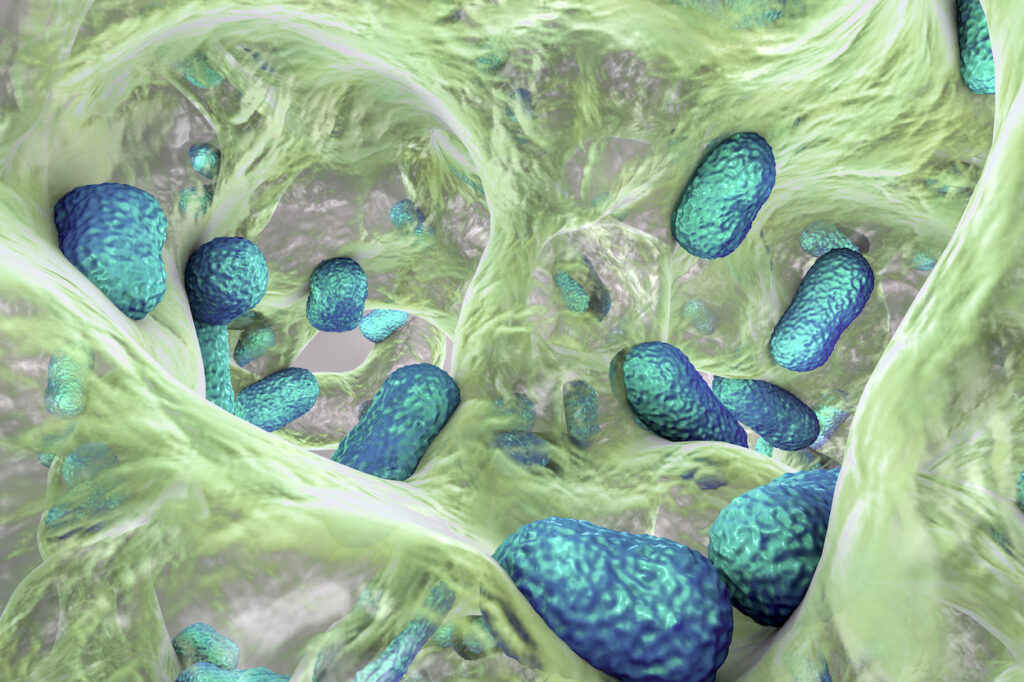
Credit: KATERYNA KON/SCIENCE PHOTO LIBRARY / Science Photo Library
In 1928, Alexander Fleming’s accidental discovery of penicillin revolutionized medicine, turning once-deadly infections into curable inconveniences. But nearly a century later, that miracle is unraveling. As antibiotic resistance (AMR) spreads, the microbes are striking back—stronger, smarter, and increasingly untreatable.
To treat bacterial infections, medical professionals prescribe antibiotics. But not all active medicine gets used up by the body. Some of it ends up in wastewater, where antimicrobial-resistant bacteria can develop. Many modern medical procedures—surgeries, chemotherapy, organ transplants, even childbirth—rely on effective antibiotics to prevent or treat infections. Without them, these procedures become dangerous or even impossible. This is why we need a novel approach to antibiotics.
To combat AMR, photopharmacology seeks to develop light-activated antimicrobials by incorporating photocages (PPGs) or molecular photoswitches into drug structures. These photoresponsive systems enable precise, noninvasive drug activation only at the infection site, minimizing environmental exposure. While photoswitches offer reversibility through light or thermal back-switching, photocaged antibiotics release the native, fully active drug upon irradiation, restoring its full antimicrobial effect.
In an ACS Central Science study titled, “Green-Light-Activatable Penicillin for Light-Dependent Spatial Control of Bacterial Growth, Biofilm Formation, and In Vivo Infection Treatment,” researchers developed and applied for the first time a green-light-activatable variant of penicillin (Penicillin-PPG).
“Controlling drug activity with light will allow precise and safe treatment of localized infections,” said Wiktor Szymanski, PhD, a corresponding author of the study from the University of Groningen. “Moreover, the fact that light comes in different colors gives us the ability to take the spatial control of drug activity to the next level.”
Light-sensitive molecules can be added to drug compounds to keep them inactive until they’re needed. Essentially, while the light molecule is attached, the functional group, such as a drug, is “caged” and cannot participate in reactions. When light shines on a modified compound, it triggers the extra molecule to break away, releasing the active drug in a process known as photocleavage. Once the target group is released, it is now free to interact or react.
The study was inspired by previous light-reactive tags, such as coumarin added to the opioid reversal agent naloxone, which requires high-energy UV or blue light to kick-start the process. However, molecular tags comprised of other coumarin compounds can be released by green light (a less intense form of light), so the team set out to develop coumarin-based modifications to create light-activated antibiotics.
After linking a coumarin-based molecule to the part of penicillin that targets bacterial cell walls (putting the antibiotic in an inert state), the researchers exposed the molecule to green light. This induces chemical rearrangement, breaking the bond and activating the penicillin.
The team demonstrates that Penicillin-PPG shows no antimicrobial activity in the dark, as well as the ability to spatially control the growth of bacteria. Initial experiments with bacteria grown in petri dishes showed that exposing the modified penicillin to green light significantly inhibited E. coli colony formation and Staphylococcus epidermidis biofilm development. Next, the researchers treated Staphylococcus aureus-infected wax moth larvae, which have immune defenses like those of humans, with an injection of the modified penicillin followed by green light therapy. Treated larvae had an improved survival rate (60%) compared to infected larvae that were left alone (30%).
The researchers added that these results are promising for future work that may expand the system to multiple light beams and different colors of light for controlling antibiotic activity in larger living organisms, including humans.
Through the application to antimicrobial drugs, perhaps the bioactivity can be regulated precisely, noninvasively, and at targeted regions in the body, simply through light irradiation. This could offer several advantages, such as achieving higher control over desired concentrations of the active drug. Additionally, this could avoid gastrointestinal side effects of the antimicrobial on the gut microbiome and reduce the buildup of active antimicrobial and the subsequent emergence of AMR in the environment.
As the antibiotic era teeters on the brink, photoresponsive antimicrobials offer a powerful new lens through which to control infection, precisely, locally, and with hope for a resistance-resilient future.