Researchers at the University of Pittsburgh have developed a new way to grow T cells in the lab that enables the cells to live longer and better destroy cancer cells in a mouse model of melanoma, compared with those cells grown using traditional growth media. T cell therapies for cancer currently rely on extensive in vitro expansion of the cells, which are then reinfused back into the body. For their study the team used the small molecule dichloroacetate (DCA) to “shift glucose usage” in the T cells during expansion, which they found improved cell metabolism, stemness and survival, and resulted in better antitumor efficacy in mice.
The findings, they suggest, could have the potential to greatly improve the effectiveness of relevant cancer immunotherapies. “The way we traditionally grow T cells in the lab is horribly inefficient,” said Greg Delgoffe, PhD, professor in the department of immunology at Pitt’s School of Medicine and director of the Tumor Microenvironment Center at UPMC Hillman Cancer Center. “We make millions of T cells and we infuse them back into a patient, but most of the cells die. Our research is uncovering new ways to manufacture T cells that live for a long time with the goal of making cell therapies more effective.”
Delgoffe is senior author of the researchers’ published paper in Cell Metabolism, titled “Redirecting glucose flux during in vitro expansion generates epigenetically and metabolically superior T cells for cancer immunotherapy.”
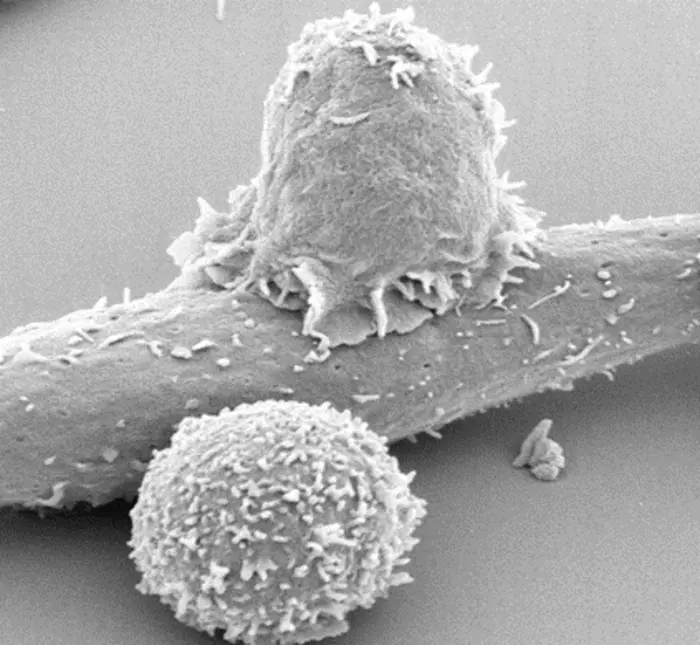
Cell therapy is a type of treatment that involves removing immune cells from the patient, expanding them in the lab and then transferring these living cells back into the patient. Common forms of adoptive cell therapy (ACT) that use T cells—the immune system’s soldiers that fight infections and cancers—include chimeric antigen receptor T cell (CAR-T) therapy, which uses T cells that have been modified to better target cancer, and tumor infiltrating lymphocyte (TIL) therapy, which uses naturally occurring T cells that can fight the tumor.
However, as the authors wrote, “A major barrier to adoptive T cell therapies is an inability to persist after infusion—a characteristic necessary for long-term efficacy.” In vivo, T cells respond to antigens and can persist an entire lifetime as memory T cells. In contrast, T cells activated in vitro only survive in culture for a few weeks, “… suggesting a large gap between the potential of T cell longevity versus what is currently possible in culture.”
Common to all forms of ACT is in vitro culture, in which mitogenic stimuli and cytokines are used to generate high numbers of tumor-reactive T cells for reinfusion, the authors continued. “The culture media used for T cell expansion has not materially changed since the mid-20th century.” They hypothesized that “… these conditions do not prepare T cells for in vivo environments, whether in the nutrient-restricted tumor or even the periphery.”
Andrew Frisch, graduate student in the department of immunology at Pitt’s School of Medicine, further explained, “Cell therapy is a living drug that responds to the environment in the body. there is a major gap between where we are with these therapies and where we could be because the way we feed these cells in the lab does not prepare them well for surviving in the body.”
According to Delgoffe, traditional growth media is very high in glucose, so T cells grown in the lab become addicted to this sugar. “In addition to mitogenic stimuli and cytokines, current in vitro culture strategies for expanding tumor-reactive T cells rely on supraphysiologic levels of glucose and other metabolites—the central idea being that ‘more is better,’” the investigators stated.
![Dr. Greg Delgoffe, professor in the Department of Immunology at the University of Pittsburgh School of Medicine and director of the Tumor Microenvironment Center at UPMC Hillman Cancer Center. [Greg Delgoffe]](https://www.genengnews.com/wp-content/uploads/2025/01/low-res-9-240x300.jpeg)
However, when reinfused into a patient, the cells struggle to consume other energy sources and most of the transferred cells quickly die. As the authors wrote, “…one major unaddressed but well-known issue is that despite the infusion of high numbers of T cells, few transferred cells can be found in circulation…Our data suggest that, despite the ability of this hypermetabolic milieu to propagate cells, it may poorly prepare lymphocytes for continued persistence in physiologic environments.”
With the goal of growing longer lasting T cells, Delgoffe, Frisch and their team supplemented a compound called dichloroacetate to the typical growth medium used to expand T cells. DCA alters the metabolism of T cells so they are less reliant on glucose and better able to use other energy sources more common in the bloodstream. “To attempt to produce more metabolically in vivo-like T cells, we used the small molecule inhibitor DCA to shift glucose usage during in vitro expansion,” they noted, explaining that, “DCA conditioning decreases reliance on glucose, promoting usage of serum-prevalent physiologic carbon sources.”
The team’s tests showed that when infused into mice, T cells grown with DCA lived much longer compared to those cells grown in traditional culture media. They found that almost one year later, over five percent of circulating killer T cells were those that had been transferred. In comparison, in mice that received T cells grown in media lacking DCA, the researchers could barely detect these cells even a few weeks later. In animals with melanoma, treatment with the DCA-grown T cells led to better tumor control and survival than with traditionally grown cells. They also provided long-lasting protection: animals that received the DCA-grown T cells fought off a second challenge with melanoma cells. “… rerouting glucose during therapeutic T cell expansion induces a metabolic phenotype allowing for superior anti-tumor activity,” the scientists stated. “Notably, treatment with DCA-expanded T cells induced strong immunologic memory in the tumor, preventing recurrence upon re-challenge with B16 melanoma several weeks after initial tumor clearance.”
Delgoffe said, “By limiting the access to certain foods, we endowed immune cells with the ability to metabolize things that they would normally metabolize in the body, rather than getting them addicted to the sugar that we were feeding them in the lab. If we can properly nourish our T cell soldiers in the lab by convincing them to eat the right kind of food, they are better prepared to respond to signals in the body and live much longer. We might be able to have a soldier on guard forever. Just as after getting the chicken pox vaccine, you are protected for life—you’ll never get chicken pox again. That’s the ultimate goal of cell therapies for cancer.”
The study results could have implications for the development of cell therapies for cancer and other diseases, the team suggested. “Collectively these findings support future in vitro strategies to modulate and imprint cells with long-lasting potency for their return to in vivo environments. This type of metabolic reprogramming may improve many types of cellular therapies beyond those for cancer, as persistence is key for success in any of these efforts.”