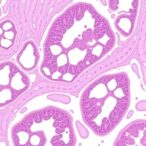
In the relentless pursuit to unravel the complex mechanisms underlying Alzheimer’s disease, a groundbreaking study has emerged, illuminating the nuanced role of apolipoprotein E (APOE) isoforms in shaping the microglial environment within the brain. These immune cells, pivotal in maintaining neural homeostasis, respond intricately to the genetic variants of APOE, a lipid-transporting protein long implicated in Alzheimer’s risk modulation. The recent research conducted by Murphy, Hu, Wolfs, and colleagues, published in Nature Communications, unveils how distinct APOE isoforms distinctly sculpt the transcriptomic and epigenomic architecture of human microglia when xenografted into an Alzheimer’s disease mouse model. This investigation offers unprecedented insight into the cellular and molecular choreography that underpins neurodegeneration, potentially steering future therapeutic strategies.
Microglia, the central nervous system’s resident immune cells, perform essential functions ranging from synaptic maintenance to response modulation against neuropathological insults. Their role in Alzheimer’s disease has gained intensified focus, especially considering their dual capacity for neuroprotection and neurotoxicity. APOE’s three major isoforms—E2, E3, and E4—manifest diverse effects on Alzheimer’s risk, with the E4 allele notably elevating susceptibility and accelerating progression. However, the mechanistic pathways through which these isoforms influence microglial behavior remained largely elusive until now.
Addressing this knowledge gap, Murphy et al. employed an innovative xenotransplantation strategy, transplanting human microglia harboring specific APOE isoforms into a mouse model genetically engineered to mimic Alzheimer’s pathology. This approach ingeniously blends human cellular biology with the in vivo complexities of neurodegeneration, circumventing limitations inherent in purely animal or in vitro systems. It allowed the researchers to observe, with precision, how APOE-dependent alterations manifest in microglial gene expression patterns and chromatin modifications within a diseased brain milieu.
Transcriptomic profiling revealed that APOE isoforms distinctly reprogram microglial gene expression. Cells expressing the E4 isoform exhibited a transcriptional signature suggestive of heightened inflammatory responsiveness and impaired metabolic regulation, aligning with the allele’s association with disease exacerbation. Conversely, E2-expressing microglia showed gene expression patterns consistent with enhanced lipid metabolism and neuroprotective functions, correlating with the allele’s protective effect against Alzheimer’s. These findings underscore a profound isoform-specific dichotomy in microglial states that may influence disease trajectory.
Equally compelling were the epigenomic insights, as the study employed state-of-the-art chromatin accessibility assays to map how APOE variants remodel microglial chromatin landscapes. The E4 microglia demonstrated widespread alterations in enhancer accessibility, particularly in genomic regions regulating immune response genes. This suggests that the deleterious effects of E4 are at least partly mediated by epigenetic reprogramming, predisposing cells toward a pro-inflammatory phenotype. This epigenomic plasticity provides a novel layer of regulatory complexity, offering potential targets for modifying microglial behavior therapeutically.
The integration of transcriptomic and epigenomic data painted a cohesive picture: APOE isoforms exert bidirectional control over microglial identity, influencing both gene expression and the underlying chromatin framework. Importantly, these molecular phenomena were observed in the context of a live brain environment experiencing Alzheimer’s pathology, thereby enhancing the physiological relevance of the findings. The humanized microglia faithfully recapitulated critical aspects of disease-associated microglial states, marking a significant advance in modeling neurodegeneration.
Moreover, the study highlighted specific transcription factors differentially engaged by APOE isoforms, mediating the observed changes in gene regulatory networks. For instance, targets of the PU.1 and IRF family transcription factors, key modulators of immune cell differentiation and activation, showed altered activity aligned with APOE-driven epigenomic remodeling. This mechanistic clarifying adds granularity to our understanding of how genetic risk converges on microglial functional shifts.
The implications of these discoveries extend beyond basic biology, informing strategies aimed at modifying microglial responses to slow or halt Alzheimer’s progression. Therapies designed to counteract the pro-inflammatory epigenomic changes induced by the APOE4 isoform could restore microglial homeostasis, mitigating neurodegeneration. Additionally, approaches enhancing the protective programs associated with APOE2 may inspire novel neuroprotective interventions.
This research also exemplifies the power of integrating multi-omics technologies with refined in vivo models. By simultaneously probing transcriptomes and epigenomes within human cells embedded in an Alzheimer’s-like environment, it sets a new standard for dissecting the gene-environment interplay in neurodegenerative disorders. Such methodological advances are critical for discovering actionable molecular targets that reflect the complexity of human brain disease.
Furthermore, the study raises intriguing questions about microglial plasticity and the potential reversibility of pathologic states. If epigenomic remodeling underlies disease-enhancing phenotypes, epigenetic editing tools might one day be harnessed to reprogram microglia therapeutically. This prospect situates the findings at the frontier of precision neuroimmunology, where genotype-informed interventions become conceivable.
Importantly, the xenograft system used in this study offers a platform for testing candidate drugs or gene therapies in a setting that mirrors the human disease context more faithfully than traditional models. This could accelerate the preclinical pipeline, enabling translational breakthroughs by validating efficacy against human microglial targets modulated by APOE variants.
The work also deepens insight into how genetic background intertwines with cellular states to influence disease. APOE’s impact on microglial identity reveals a critical axis by which inherited risk factors manifest phenotypically within the immune compartment of the brain. This adds a layer of complexity to Alzheimer’s pathophysiology that must be considered when developing biomarkers or stratifying patients based on genotype.
While this study focuses on microglia, its mechanistic revelations likely extend to other glial populations, such as astrocytes and oligodendrocytes, which interact intimately with microglia during neurodegeneration. Future research will inevitably expand on how APOE isoforms orchestrate broader glial networks, further illuminating the cellular ecosystem driving Alzheimer’s disease.
In sum, Murphy, Hu, Wolfs, and colleagues have delivered a landmark exploration of the molecular underpinnings by which APOE isoforms influence microglia within the Alzheimer’s brain. Their multi-dimensional characterization of transcriptomic and epigenomic landscapes not only advances fundamental neuroscience but also opens new avenues for targeted therapeutic innovation. As the field moves toward precision medicine in neurodegeneration, such integrative studies will be paramount in turning genetic insights into tangible clinical advances.
Subject of Research:
The differential impact of APOE isoforms on the transcriptomic and epigenomic landscapes of human microglia in an Alzheimer’s disease context.
Article Title:
The APOE isoforms differentially shape the transcriptomic and epigenomic landscapes of human microglia xenografted into a mouse model of Alzheimer’s disease.
Article References:
Murphy, K.B., Hu, D., Wolfs, L. et al. The APOE isoforms differentially shape the transcriptomic and epigenomic landscapes of human microglia xenografted into a mouse model of Alzheimer’s disease. Nat Commun 16, 4883 (2025). https://doi.org/10.1038/s41467-025-60099-4
Image Credits: AI Generated
Tags: Alzheimer’s risk factors and geneticsAPOE isoforms in Alzheimer’s diseaseepigenomic architecture of microgliaimmune cells in brain healthlipid-transporting proteins in neurodegenerationmicroglial function in neuroinflammationmicroglial response to APOE variantsneurodegeneration mechanismsneuroprotection and neurotoxicity in Alzheimer’sresearch on Alzheimer’s mouse modelstherapeutic strategies for Alzheimer’stranscriptomic changes in microglia