In recent years, the landscape of cancer treatment has been dramatically transformed by the advent of immune checkpoint inhibitors (ICIs), therapies that empower the immune system to recognize and eradicate tumor cells. However, despite the revolutionary potential of ICIs, their efficacy is limited to only a subset of patients, highlighting the urgent need for reliable biomarkers that predict treatment responses. A novel study published in the June 2025 issue of Oncotarget delves into the multifaceted role of the CHEK2 gene in solid tumors, presenting compelling evidence that extends beyond its classical function in DNA damage repair to encompass significant immunomodulatory properties that may shape tumor response to immunotherapy.
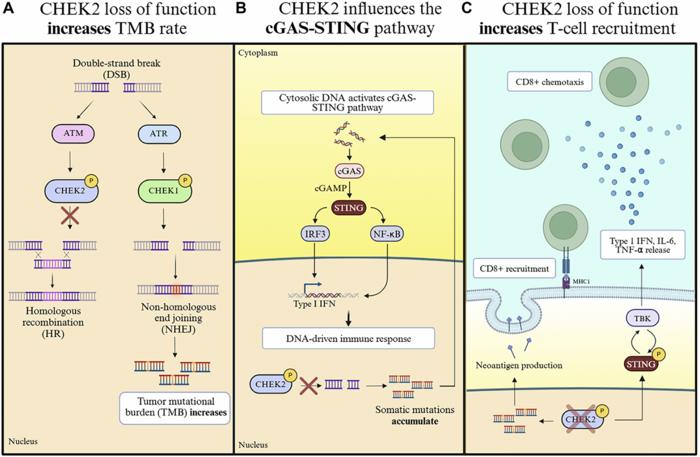
CHEK2, widely recognized as a key player in the DNA damage response (DDR) pathway, traditionally functions as a tumor suppressor by orchestrating precise repair mechanisms following double-stranded DNA breaks. Specifically, CHEK2 facilitates homologous recombination (HR), an error-free repair pathway crucial for maintaining genome stability. Loss of CHEK2 function disrupts this precise repair system, forcing cells to compensate by resorting to the more error-prone non-homologous end joining (NHEJ) pathway. This shift not only leads to the gradual accumulation of somatic mutations but also increases tumor mutational burden (TMB), a factor increasingly correlated with better immunotherapy outcomes due to the generation of neoantigens recognizable by immune cells.
The new review, spearheaded by researchers from Northwestern University Feinberg School of Medicine, highlights a dual mechanism whereby CHEK2 deficiency potentially amplifies anti-tumor immune responses. First, the elevated mutational burden arising from deficient HR repair generates an array of neoantigens, alerting cytotoxic T cells (especially CD8+ subsets) to the presence of malignant cells. Second, and perhaps more intriguingly, the review elucidates the role of the cyclic GMP-AMP synthase (cGAS)-stimulator of interferon genes (STING) pathway as a secondary mechanism influenced by CHEK2 loss. DNA fragments generated by inaccurate repair escape the nucleus, accumulating in the cytosol where cGAS recognizes them as aberrant. This recognition activates the STING pathway, triggering a cascade that culminates in the production of Type I interferons and chemotactic cytokines, fostering a pro-inflammatory microenvironment conducive to robust T cell recruitment.
.adsslot_xu5sSTgcf6{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_xu5sSTgcf6{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_xu5sSTgcf6{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
This intricate interplay between deficient DNA repair and innate immune activation elucidates why CHEK2-deficient tumors may demonstrate heightened infiltration of immune effectors. Notably, in cancers traditionally resistant to ICIs, such as glioblastoma and renal cell carcinoma, reduced CHEK2 expression correlated with increased CD8+ T cell presence and elevated expression of interferon-stimulated genes. These findings hint at the immunomodulatory potential of CHEK2 as not merely a bystander but an active participant in shaping the immune landscape of solid tumors, altering the paradigm by which tumor immunogenicity is understood.
Moreover, the research underscores the translational potential of these insights through examples of clinical investigations employing CHEK inhibitors alongside ICIs. Prexasertib, a dual CHEK1/2 inhibitor, has surfaced in early-stage trials demonstrating promising synergistic effects with PD-1 blockade. These preliminary data suggest that pharmacological inhibition of CHEK2 might potentiate immune activation within the tumor microenvironment, potentially sensitizing otherwise refractory cancers to immunotherapy.
The broader implications of this review extend to the identification of CHEK2 as a biomarker with prognostic and predictive utility. Determining CHEK2 status in patients could refine immunotherapy stratification, enabling clinicians to pinpoint those most likely to benefit from checkpoint blockade. This capability would represent a significant stride toward personalized cancer treatment, optimizing therapeutic outcomes while minimizing unnecessary exposure to ineffective modalities.
Fundamentally, this research enriches our understanding of the crosstalk between DNA repair pathways and immune regulation. The prevailing view perceives DDR genes as guardians of genome integrity alone; however, CHEK2 emerges as a bridge linking genomic instability to immune activation. By dictating the balance between error-free and error-prone repair, CHEK2 indirectly governs the generation of cytosolic DNA fragments that stimulate innate immune pathways, illustrating an elegant feedback mechanism that could be leveraged therapeutically.
The authors also address the complexities inherent in targeting CHEK2, not least the duality of its functions. While loss of CHEK2 augments immune visibility by increasing mutation-derived neoantigens and activating cGAS-STING signaling, complete inhibition might also exacerbate genomic instability with unpredictable consequences. Therefore, therapeutic strategies demand cautious design, possibly integrating precise dosing regimens or combinatory approaches that engage multiple aspects of tumor biology and immune regulation.
This review invites further inquiry into the molecular nuances of CHEK2’s immunomodulatory roles. Delineating the temporal dynamics of cGAS-STING activation in response to DNA damage and the interplay with other immune checkpoints could unravel additional layers of regulation. Moreover, exploring the heterogeneity across tumor types in CHEK2 expression and function might reveal subtype-specific vulnerabilities, tailoring interventions even further.
Beyond the laboratory, these findings resonate with ongoing clinical efforts to overcome cancer’s notorious evasiveness. By illuminating the nexus between defective DNA repair and immune activation, the study paves the way for innovative combination therapies that exploit intrinsic tumor weaknesses. As such, it reinforces the concept that successful immunotherapy requires not only immune targeting but also strategic modulation of tumor biology to unlock the immune system’s full potential.
In conclusion, the emerging paradigm positions CHEK2 as a pivotal molecular switch at the crossroads of DNA repair and immune surveillance. Harnessing this dual functionality holds the promise of enhancing immunotherapy efficacy and expanding treatment horizons for patients with solid tumors. As research advances, the integration of CHEK2 status evaluation and CHEK-targeted therapies may redefine cancer management, exemplifying the power of translational science to transform patient outcomes.
Subject of Research: Cells
Article Title: Beyond DNA damage response: Immunomodulatory attributes of CHEK2 in solid tumors
News Publication Date: 10-Jun-2025
Web References:
https://www.oncotarget.com/archive/v16/
http://dx.doi.org/10.18632/oncotarget.28740
Image Credits: Copyright © 2025 Qian et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
Keywords: cancer, CHEK2, immune checkpoint inhibitors, immunomodulation
Tags: biomarkers for immunotherapy responsecancer treatment advancementsCHEK2 gene role in cancerDNA damage repair mechanismsenhancing immunotherapy efficacyhomologous recombination in cancerimmune checkpoint inhibitors in solid tumorsimmunomodulatory properties of CHEK2non-homologous end joining pathwaysolid tumor immunotherapy strategiestumor mutational burden significancetumor suppressor functions of CHEK2