A groundbreaking study emerging from Japan’s serene rural landscapes challenges conventional wisdom regarding “normal” blood glucose levels and their influence on long-term mortality risks. While managing blood glucose to prevent diabetes has been a global health priority for decades, new research underscores the subtler intricacies within glucose regulation that could reshape how clinicians approach patient care. The decades-spanning Ohasama Study, conducted in a small farming town in the Tohoku Region, has unearthed compelling associations between one-hour post-glucose load blood sugar levels and survival rates, even among individuals without diabetes.
The Ohasama Study’s longitudinal approach, initiated in the 1980s in Iwate Prefecture, involves comprehensive health evaluations of local inhabitants, capturing extensive physiological data across multiple generations. Central to this research is the oral glucose tolerance test (OGTT), a diagnostic cornerstone wherein participants ingest a glucose solution, and their blood sugar responses are measured at baseline and subsequent intervals. By tracing these glucose fluctuations every four years, researchers have generated a rich dataset that reveals not only the progression towards diabetes but also nuanced links between glucose dynamics and mortality.
Led by notable researchers Junta Imai and Hideki Katagiri at Tohoku University, alongside collaborators from several Japanese medical institutions, the investigation delved into nearly a millennium of participants. The team scrutinized various health markers but pinpointed the one-hour post-glucose load blood glucose level as a remarkably potent predictor of risk. Crucially, this correlation persisted even after statistically controlling for confounding factors such as age, smoking status, and body mass index, indicating an independent and robust relationship between postprandial glucose spikes and overall mortality.
.adsslot_H0a7M93Gqy{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_H0a7M93Gqy{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_H0a7M93Gqy{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
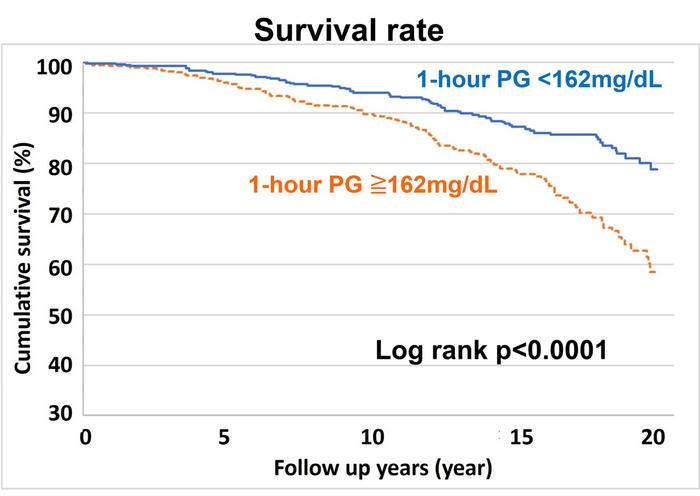
To parse these findings with greater precision, participants were stratified based on their median glucose levels measured one hour after glucose intake, set at a threshold of 162 mg/dL. Survival analyses vividly demonstrated that individuals maintaining glucose levels below this benchmark enjoyed superior longevity compared to those exceeding it. To refine these insights, the study further concentrated on 595 subjects exhibiting normal glucose tolerance—essentially excluding diabetes cases—to focus on subtler glucose variations within the conventional healthy range.
Within this refined cohort, statistical exploration identified 170 mg/dL as the pivotal one-hour glucose concentration that most powerfully forecasted mortality outcomes. Over two decades, survival rates starkly diverged: nearly four out of five individuals with glucose levels below 170 mg/dL remained alive, contrasting sharply with a mortality rate approaching 50% in those surpassing this level. The stark dichotomy elucidates how even moderate postprandial glucose elevations, previously considered clinically insignificant, may foreshadow grave health consequences.
Beyond overall mortality, the study dissected cause-specific death data, exposing a significantly elevated risk among higher-glucose individuals for heart diseases rooted in atherosclerosis. This insinuates that transient glucose surges could accelerate vascular inflammation and plaque development, thereby exacerbating cardiovascular risks. Additionally, deaths attributed to malignant tumors were disproportionately higher in this group, suggesting a possible mechanistic link between glucose metabolism and cancer progression, possibly through pathways involving insulin resistance, oxidative stress, or chronic low-grade inflammation.
These revelations inject a critical perspective into the prevailing understanding of glucose homeostasis, challenging the adequacy of existing “normal” diagnostic thresholds. Blood glucose is traditionally evaluated through fasting measurements or two-hour post-load values; however, the one-hour post-load reading may serve as a more sensitive biomarker for identifying individuals at heightened risk long before overt diabetes manifests. Such an approach could revolutionize preventative strategies by targeting earlier metabolic disturbances instead of waiting for threshold-crossing diagnoses.
The implications of this research resonate far beyond Ohasama’s rural boundaries. If these findings are replicated across diverse populations, they could necessitate a paradigm shift in clinical practice. Healthcare providers might increasingly incorporate one-hour postprandial glucose assessments into routine screenings, empowering early interventions aimed at modulating post-meal glucose spikes through dietary modifications, pharmacological agents, or lifestyle adjustments. This proactive stance could mitigate vascular and oncologic morbidity and mortality on a population scale.
Furthermore, the Ohasama Study’s enduring contribution exemplifies the unparalleled value of long-term, community-centered epidemiological research. By patiently amassing detailed biomedical data spanning decades, the study uncovers patterns imperceptible in shorter investigations. Such comprehensive surveillance illuminates subtle physiological dynamics that hold profound prognostic significance, emphasizing that quiet rural regions can yield insights crucial to the global battle against chronic diseases.
The study also elegantly underscores the complexity of blood glucose regulation. Glucose excursions—those rapid rises following carbohydrate ingestion—may exert outsized impacts on endothelial function, oxidative stress, and inflammatory signaling pathways. Understanding these intricate biochemical cascades invites the development of refined therapeutic targets beyond fasting glucose reduction, honing in on glycemic variability as a modifiable risk factor.
Parallel to its scientific insights, this research carries compelling public health messages. Individuals, even those currently deemed healthy by standard metrics, might benefit from heightened awareness and proactive management of postprandial glucose levels. Nutritional counseling emphasizing low-glycemic-index foods, physical activity to enhance insulin sensitivity, and potentially novel glucose-modulating drugs could collectively form pillars of a preventative healthcare approach informed by cutting-edge science.
In sum, the Ohasama Study delivers profound evidence that the story of blood glucose and mortality is far more nuanced than previously imagined. The revelation that relatively modest post-load glucose levels predict cardiovascular and cancer-related deaths reshapes foundational concepts in metabolic health. This invites a future where earlier, more precise interventions curtail disease trajectories, extend longevity, and foster healthier aging societies worldwide. As science continues unraveling the complexities of human metabolism, the humble one-hour glucose test emerges as a vital tool unlocking lifesaving potential.
Subject of Research: The relationship between one-hour post-glucose load blood glucose levels and long-term mortality risk from cardiovascular diseases and malignant neoplasms in individuals without diabetes.
Article Title: One-hour post-load glucose levels predict mortality from cardiovascular diseases and malignant neoplasms in healthy subjects
News Publication Date: 2-Jun-2025
Web References: http://dx.doi.org/10.1093/pnasnexus/pgaf179
Image Credits: Junta Imai et al.
Keywords: Diabetes, Blood Glucose, Cardiovascular Disease, Cancer, Mortality, Glucose Tolerance Test, Postprandial Glucose, Epidemiology, Metabolic Health
Tags: clinical implications of glucose levelsdiabetes prevention strategieselevated blood glucose levelsglucose dynamics and survivalglucose regulation and longevityJapan Tohoku Region health studylong-term mortality risksOhasama Study findingsoral glucose tolerance testphysiological data across generationspost-glucose load blood sugarrural health research Japan