In the ever-evolving landscape of gastrointestinal surgery, one of the most persistent and vexing complications is the development of postoperative intestinal anastomotic fistulas (PIAF). These abnormal connections, forming at the surgical joining sites of the intestine, pose a significant threat to patient recovery due to their high morbidity and complex management needs. Traditional treatment modalities have offered inconsistent outcomes, often accompanied by prolonged hospital stays and additional interventions. However, a groundbreaking retrospective study now shines a beacon of hope by demonstrating the efficacy of endoscopic purse-string suturing (EPS) as a minimally invasive rescue strategy for these challenging cases.
Over nearly a decade-long analysis spanning from 2015 to 2024, researchers examined 55 patients suffering from refractory PIAF who underwent EPS at a renowned gastrointestinal center. This technique leverages an endoscope-equipped purse-string suture to mechanically close fistulas, thereby promoting tissue healing without the need for extensive surgical re-exploration. Importantly, the study’s dual focus on both technical and clinical success provides crucial insights into the practical viability and long-term benefits of this innovative approach.
The technical success rate of EPS in this cohort stood impressively at 87.3%, suggesting that the majority of fistulas could be effectively sealed endoscopically. Nevertheless, clinical success—defined by confirmed healing through imaging and endoscopic evaluation—was achieved in 63.6% of cases. While these figures represent a marked improvement over conventional therapies, they also underscore the complexity inherent to managing fistulas resistant to initial treatment attempts.
Critically, the research identified no statistically significant differences in outcomes between patients referred internally within the healthcare system and those referred externally. This finding not only attests to the reproducibility of EPS across varied patient populations and referral sources but also signals the potential for widespread adoption of this modality in diverse clinical settings.
One particularly intriguing aspect of the study centers on the role of preoperative ostomy status. Patients who underwent ostomy creation prior to EPS enjoyed higher clinical success rates—an impressive 92.3%—compared to those without ostomies, whose success rate was closer to 54.8%. This observation invites further investigation into the protective or preparatory benefits that ostomies might confer, perhaps by diverting fecal flow and reducing local contamination at the anastomotic site.
Timing emerged as another pivotal factor influencing treatment outcomes. Multivariate logistic regression analysis pinpointed delayed intervention—defined as over two months post-fistula diagnosis—as a strong independent risk factor for poor prognosis. Those who received EPS within the early disease course fared substantially better, emphasizing the critical window in which minimally invasive intervention can be most efficacious.
Additionally, the presence of pre-existing anastomotic strictures—a narrowing of the intestinal lumen caused by fibrosis or inflammation—was associated with diminished clinical success. Strictures likely impede both mechanical closure and subsequent tissue healing, posing a formidable obstacle in fistula resolution and highlighting the need for tailored strategies in such scenarios.
From a safety standpoint, the endoscopic purse-string technique demonstrated a commendable profile. Only a minority of patients experienced complications, with anastomotic stricture occurring in 3.6% of cases, all manageable via further endoscopic procedures. Transient diarrhea was reported in one individual, but no mortality or fistula recurrence was observed during a rigorous twelve-month follow-up period. These findings underscore both the minimally disruptive nature of EPS and its durability as a treatment option.
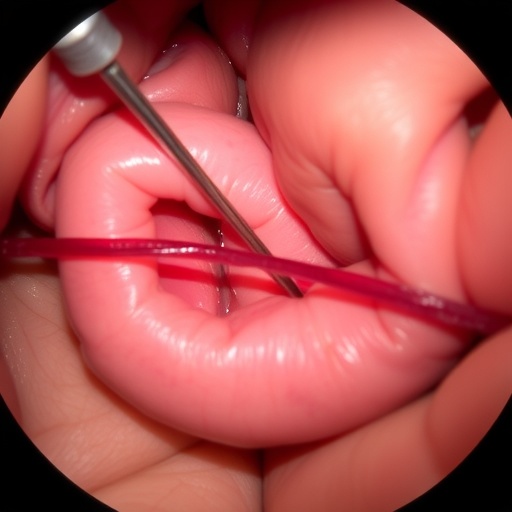
The technical underpinnings of the EPS procedure involve maneuvering an endoscope equipped with specialized suturing devices to encircle the fistula’s orifice meticulously. By tightening the purse-string suture, the fistular opening is constricted, which promotes granulation tissue formation and eventual sealing. This technique exemplifies how advancements in endoscopic instrumentation can translate into real-world clinical solutions for notoriously intractable surgical complications.
Furthermore, the study accentuates the imperative of ‘time-sensitive intervention’—the concept that early, proactive management significantly alters the trajectory of complicated intestinal healing. Waiting beyond a two-month threshold not only compromises the likelihood of fistula closure but may also necessitate more invasive reconstructive surgeries with attendant risks.
In addition to temporal considerations, patient selection criteria remain paramount. The data advocates for selective stoma creation pre-EPS, suggesting that this adjunctive step can optimize the intestinal environment for healing. This multifaceted approach integrates surgical planning with innovative endoscopic therapy, reflecting a holistic strategy in complex fistula management.
Notably, the findings have profound implications for current clinical guidelines, potentially redefining standard care pathways for refractory PIAF. As minimally invasive techniques continue to supplant more aggressive surgeries, EPS may emerge as a frontline rescue therapy, minimizing patient morbidity and healthcare costs while accelerating recovery.
While the retrospective nature of the study invites cautious interpretation, its robust sample size and comprehensive follow-up set a new benchmark in the field. Future prospective randomized trials could further validate these promising results and explore refinements such as adjunctive agents to bolster tissue healing or novel suture materials enhancing biocompatibility.
In a broader context, the success of EPS underscores the transformative potential of endoscopic innovations in gastrointestinal surgery. By converting what was once a dreaded, often devastating postoperative complication into a manageable condition through internal suturing, this technique aligns with the ongoing paradigm shift toward minimally invasive, patient-centric care models.
As surgeons and gastroenterologists embrace endoscopic tools not merely for diagnostics but for definitive therapeutics, the case of EPS in refractory PIAF exemplifies innovation meeting clinical necessity. It also opens avenues for analogous applications in other fistulous and perforative pathologies within the alimentary tract and beyond.
Ultimately, this research resonates beyond the technical specifics, embodying a narrative of surgical progress that marries precision engineering with compassionate patient care. The endoscopic purse-string suture is poised to rewrite the script of postoperative intestinal leaks, transforming a formidable challenge into a triumph of modern medicine.
—
Subject of Research: Postoperative intestinal anastomotic fistula (PIAF) management using endoscopic purse-string suturing (EPS)
Article Title: Clinical application of “purse-string suture” under endoscope in the treatment of refractory postoperative intestinal anastomotic fistula
Article References:
Zhu, G., Zhou, S., Gao, H. et al. Clinical application of “purse-string suture” under endoscope in the treatment of refractory postoperative intestinal anastomotic fistula. BMC Cancer 25, 931 (2025). https://doi.org/10.1186/s12885-025-14364-w
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14364-w
Tags: clinical outcomes in fistula managementendoscopic purse-string suturingendoscopic techniques in surgerygastrointestinal complications managementinnovative surgical approachesminimally invasive gastrointestinal surgerypatient recovery in gastrointestinal surgerypostoperative intestinal anastomotic fistulasrefractory fistulas treatmentretrospective study on fistula healingtechnical success in endoscopytissue healing methods