Sepsis remains one of the most daunting challenges in modern critical care medicine, posing a significant mortality risk among intensive care unit (ICU) patients worldwide. This complex syndrome, resulting from the body’s extreme response to infection, often culminates in multi-organ failure, necessitating precise clinical tools to evaluate and monitor patient status effectively. Central to this endeavor is the Sequential Organ Failure Assessment (SOFA) score, a clinical scoring system that quantitatively measures the extent of organ dysfunction across multiple systems. The development and widespread adoption of the SOFA score marked a transformative step in sepsis diagnosis and management, becoming an integral element of the Sepsis-3 consensus criteria and a pivotal guide for therapeutic decision-making.
The original SOFA score, established over a decade ago, assesses six organ systems—respiratory, cardiovascular, hepatic, coagulation, renal, and neurological—to produce a composite score indicating severity of organ failure. A rise of two or more points signals significant organ dysfunction and correlates with increased mortality risk. In response to evolving critical care practices including newer organ-support modalities and pharmacologic agents, a revised iteration, SOFA-2, has recently been proposed. This update aimed to recalibrate score components, adjust thresholds based on contemporary mortality data, and incorporate advances in ICU therapeutics to enhance accuracy and clinical relevance.
Despite the conceptual advances underpinning SOFA-2, questions remained unanswered regarding its performance specifically in sepsis patients, who represent a distinct subset with unique pathophysiological and clinical characteristics. Validation in a broad ICU cohort had been undertaken, but the nuanced dynamics of sepsis called for targeted examination. This knowledge gap held substantial implications as any significant divergence in performance could potentially alter sepsis identification, severity stratification, and ultimately impact patient management guidelines worldwide.
Addressing this critical question, a team of researchers at the First Affiliated Hospital of Sun Yat-Sen University in Guangzhou, China, embarked on the first comprehensive validation of SOFA-2 within a rigorously defined sepsis cohort. This effort leveraged data from the TESTS trial—a large, multicenter randomized controlled trial focusing on adults diagnosed with sepsis according to Sepsis-3 criteria. Utilizing such a meticulously adjudicated clinical trial database confers higher fidelity to sepsis diagnoses than retrospective studies dependent on electronic health record abstraction.
The study cohort comprised 1,089 adult sepsis patients, presenting a median age of 64.5 years, with females accounting for just over 31% of participants. The ICU mortality rate in this group was noted to be 9.2%, reflecting the significant lethality of sepsis. The investigators recalculated both the original SOFA (SOFA-1) and the updated SOFA-2 scores at the time of patient randomization, scrutinizing their distributions as well as the ability to discriminate between survivors and non-survivors in the ICU setting.
Interestingly, the SOFA-2 scores were modestly lower on average compared to the SOFA-1 scores, with median values of 6 versus 7 respectively. Analyses suggested that these differences stemmed mainly from adjustments in respiratory, cardiovascular, and hepatic components, whereas the renal sub-score exhibited a tendency toward higher values in SOFA-2. Despite these shifts, the concordance between the two scoring systems was remarkably close, especially at clinically critical thresholds. Notably, only 2.2% of patients who met the two-point organ dysfunction threshold under SOFA-1 failed to meet it under SOFA-2, implying minimal impact on sepsis classification from the updated scoring.
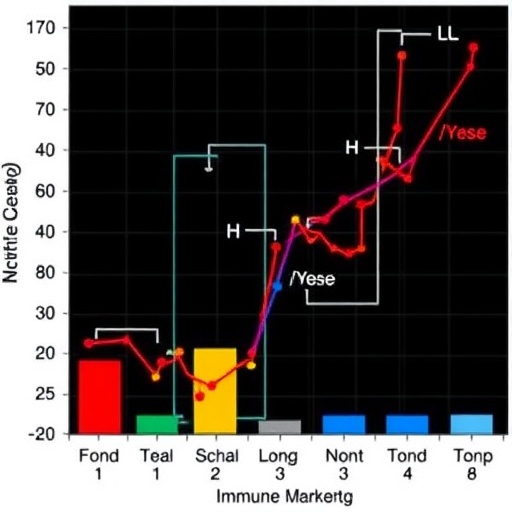
Beyond distributional analysis, the diagnostic specificity of the two scores was found to be nearly indistinguishable when predicting ICU mortality. The area under the receiver operating characteristic curve (AUROC), a standard metric of discriminative performance, was 0.646 for SOFA-2 and 0.641 for SOFA-1. Comparable results were obtained for mortality endpoints at 28 days and 90 days, suggesting that despite technical updates, SOFA-2 preserves the essential clinical prognostic signal upon which critical care clinicians depend. It is important to emphasize that the SOFA score was never intended as a pure mortality prediction tool but remains closely linked to patient outcomes via the severity of organ failure it captures.
Recognizing that immune dysregulation is a fundamental driver of sepsis pathogenesis, the researchers further explored whether augmenting SOFA-2 with additional immune markers might bolster its predictive power. The SOFA-2 design omitted an immunologic domain on the premise that routinely available immune metrics, such as white blood cell and lymphocyte counts, are inadequate surrogates for sepsis immune status. Employing advanced machine learning techniques, the study evaluated five immune-related indicators measurable in the dataset—white blood cell count, lymphocyte count, monocyte HLA-DR expression, neutrophil-to-lymphocyte ratio, and regulatory T-cell percentage—across various combined models.
Contrary to expectations, none of these immune parameters significantly enhanced the score’s discrimination between survivors and non-survivors. This finding underscores the profound biological complexity and heterogeneity of immune dysfunction in sepsis, which is highly dynamic and not easily encapsulated by static baseline laboratory measurements. The inability of simplistic immune markers to confer incremental predictive value illustrates the formidable challenge in integrating immunological dimensions into practical bedside scoring systems designed for rapid clinical use.
Taken collectively, the study represents a landmark in validating the updated SOFA-2 score in sepsis patients, confirming that this contemporary revision maintains clinical continuity with its predecessor while adapting to modern ICU realities. The results support ongoing adoption of SOFA-2 in both clinical and research contexts pertaining to sepsis care. Simultaneously, the work highlights intrinsic limitations in capturing sepsis immune dysregulation through conventional markers, signaling the need for richer, more sophisticated biomarkers and dynamic assessment strategies in future sepsis severity scoring models.
The research was led by Qingui Chen, Associate Research Fellow and PhD advisor specializing in clinical and translational critical care research with expertise in big data analytics, alongside Jianfeng Wu, a prominent Professor and PhD Supervisor with extensive publications in top-tier international journals and leadership roles in Chinese critical care medicine. Their collaborative efforts advance understanding of sepsis assessment and pave a promising path for integrating evolving clinical insights into improved patient management worldwide.
Ultimately, this investigation illuminates the balance between maintaining established clinical tools and the imperative for iterative refinement in an era of rapid medical innovation. SOFA-2’s validation in sepsis not only ensures fidelity to foundational diagnostic criteria but also reflects a steadfast commitment to evidence-based evolution in critical care scoring systems—a vital underpinning for progress against one of medicine’s most formidable adversaries.
Subject of Research: Validation of the updated SOFA-2 score specifically in sepsis patients and the exploration of immune biomarker incorporation to enhance predictive performance.
Article Title: Validation of SOFA-2 score in sepsis and exploration of its extension with additional immune markers
News Publication Date: January 8, 2026
Web References: http://dx.doi.org/10.1016/j.jointm.2025.12.003
Image Credits: Prof. Wu Jianfeng from Sun Yat-Sen University, Guangzhou, China
Keywords: Health and medicine, Clinical medicine, Health care, Human health, Sepsis, Diseases and disorders, Septic shock, Medical diagnosis, Clinical studies, Human biology
Tags: clinical tools for patient evaluationcontemporary ICU therapeuticscritical care medicine advancementsmortality risk assessment in sepsismulti-organ failure in ICUorgan dysfunction scoring systemspredictive power of immune markerssepsis diagnosis and managementSepsis-3 consensus criteriaSequential Organ Failure AssessmentSOFA-2 score in sepsisupdated SOFA score components