In the intricate landscape of inflammatory bowel disease (IBD), a spectrum of cellular and molecular disruptions converge to elicit chronic inflammation and tissue damage. Among the multifaceted contributors to IBD pathology, reactive oxygen species (ROS) have long stood out for their dual role in cellular signaling and oxidative injury. While elevated ROS levels are emblematic of IBD, attempts to broadly quell these reactive molecules using general antioxidants have delivered disappointing therapeutic results, underscoring the need for more precise molecular interventions. A recent study published in Nature Metabolism now illuminates a novel mechanistic axis implicating lipid metabolism within intestinal fibroblasts as a critical regulator of epithelial cell fate, thereby reshaping our understanding of epithelial vulnerability in the context of IBD.
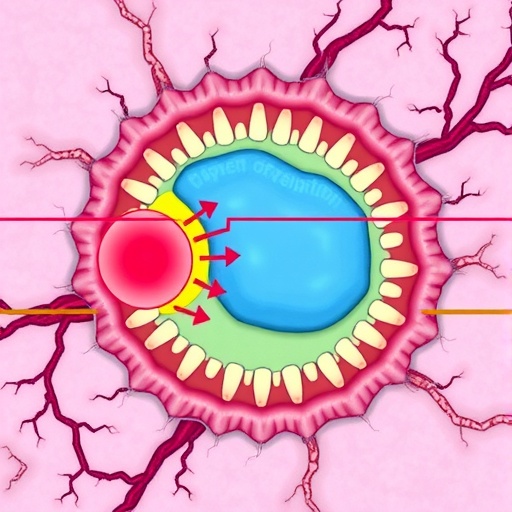
The study spearheaded by Huang, Zhang, Das, and colleagues unveils a sophisticated interplay between fibroblast lipid metabolism and epithelial susceptibility to an iron-dependent form of programmed cell death known as ferroptosis. Ferroptosis, distinguished from apoptosis and necrosis by its reliance on iron-catalyzed lipid peroxidation, emerges as a pivotal driver of epithelial cell loss in chronic intestinal inflammation. By delving deeply into cell-type-specific metabolic dynamics, the researchers pinpointed the acyl-CoA synthetase long-chain family member 4 (ACSL4) as a linchpin enzyme whose expression in fibroblasts profoundly influences epithelial stability.
Fibroblasts, often overshadowed by immune and epithelial cells in IBD research, assume center stage in this investigation. The team demonstrated that in both human IBD tissues and murine models of chronic colitis, ACSL4 is markedly overexpressed in intestinal fibroblasts. This elevation is not a mere epiphenomenon; rather, it rewires fibroblast lipid metabolic pathways, thereby orchestrating a microenvironment predisposed to ferroptosis in adjacent epithelial cells. Such heterocellular crosstalk reveals a previously unappreciated mechanism whereby fibroblasts modulate epithelial cell death indirectly through metabolic mediation.
.adsslot_RLdMxwa2BC{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_RLdMxwa2BC{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_RLdMxwa2BC{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Functionally, fibroblast-specific overexpression of ACSL4 exacerbates intestinal damage by amplifying epithelial ferroptosis, intensifying the inflammatory milieu, and worsening disease severity in mouse models. Conversely, abrogation of ACSL4 activity within fibroblasts—achieved either pharmacologically or via genetic deletion—significantly ameliorates colitis symptoms. This dual approach highlights ACSL4 not only as a biomarker of disease progression but also as a promising therapeutic target capable of disrupting the pathogenic cascade at its nexus.
At the biochemical level, ACSL4 catalyzes the ligation of long-chain polyunsaturated fatty acids to coenzyme A, facilitating their incorporation into cellular membranes as phospholipids. The enrichment of susceptible lipid species in the fibroblast milieu enhances the generation of lipid hydroperoxides under oxidative stress conditions, priming neighboring epithelial cells for ferroptotic demise. This mechanistic insight elucidates why broad-spectrum ROS inhibition fails clinically: the spatial and molecular specificity of lipid peroxidation in the fibroblast-epithelial axis demands more nuanced intervention strategies.
The implications of this work ripple beyond the confines of IBD pathology, touching on the broader paradigm of how stromal cells influence epithelial integrity through metabolic remodeling. The discovery that fibroblast lipid metabolism shapes epithelial cell fate adds complexity to how we view tissue homeostasis and injury in chronic inflammatory states. It challenges researchers to consider stromal metabolic pathways as integral to disease emergence and as underexplored reservoirs of therapeutic opportunity.
This study also reinvigorates interest in ferroptosis as a disease mechanism, which until recently has been primarily investigated within cancer biology and neurodegeneration. The demonstration of ferroptosis in the intestinal epithelium as a contributor to chronic inflammation and tissue destruction broadens the clinical relevance of ferroptotic pathways. It also suggests that ferroptosis inhibitors, some of which are in early-stage development for other indications, might find new application in IBD treatment paradigms.
Moreover, the elucidation of ACSL4’s role within fibroblasts reframes the controversy surrounding antioxidant therapies in IBD. By illuminating the selective lipid metabolic processes underlying ferroptotic sensitivity, the study advocates for a targeted approach over generalized ROS scavenging. This precision approach may overcome the limitations of previous antioxidant trials that lacked molecular specificity and resulted in suboptimal clinical outcomes.
From a translational viewpoint, the identification of fibroblast ACSL4 as a driver of epithelial ferroptosis opens avenues for biomarker development, enabling clinicians to stratify patients based on stromal metabolic activity. This stratification could guide personalized therapeutic regimens, integrating ferroptosis inhibition alongside conventional anti-inflammatory and immunosuppressive agents. Such integrative strategies promise to enhance treatment efficacy while potentially minimizing systemic side effects.
In probing the heterocellular metabolic crosstalk, the research invites further questions concerning the upstream triggers for ACSL4 upregulation in fibroblasts. Is this altered metabolic state a response to inflammatory cues, intrinsic fibroblast activation states, or microenvironmental factors such as hypoxia or microbiota-derived metabolites? Deciphering these upstream regulators could reveal yet more precise intervention points to intercept pathological fibroblast reprogramming before epithelial injury ensues.
Furthermore, the bidirectional communication between fibroblasts and epithelial cells underscores the complexity of gut microenvironments in chronic disease. The study’s findings emphasize that targeting epithelial cells alone may be insufficient; instead, therapeutics must account for stromal contributions that dynamically affect epithelial susceptibility to damage. The fibroblast-centric focus thus enriches the conceptual framework for IBD pathogenesis and therapeutic design.
The utilization of sophisticated mouse models that recapitulate chronic colitis and human tissue analyses strengthens the biological relevance and translational potential of the findings. By verifying ACSL4’s overexpression and functional impact across species and disease contexts, the research solidifies the clinical significance of the fibroblast-epithelial ferroptosis axis.
In summary, the discovery of ACSL4’s pivotal role in fibroblast-mediated regulation of epithelial ferroptosis represents a paradigm shift in IBD biology. It integrates metabolic reprogramming within stromal cells into the broader narrative of inflammatory epithelial injury, offering a compelling mechanistic explanation for epithelial vulnerability amid oxidative stress. This insight charts a strategic path toward targeted antioxidant therapies, aiming to disrupt ferroptotic pathways with clinical precision and heralds a new era of metabolism-based interventions in chronic intestinal inflammation.
Subject of Research: Inflammatory bowel disease (IBD), ferroptosis, lipid metabolism, acyl-CoA synthetase long-chain family member 4 (ACSL4), intestinal fibroblast-epithelial crosstalk
Article Title: Fibroblast lipid metabolism through ACSL4 regulates epithelial sensitivity to ferroptosis in IBD
Article References:
Huang, W., Zhang, Y., Das, N.K. et al. Fibroblast lipid metabolism through ACSL4 regulates epithelial sensitivity to ferroptosis in IBD. Nat Metab (2025). https://doi.org/10.1038/s42255-025-01313-x
Image Credits: AI Generated
Tags: acyl-CoA synthetase long-chain familycellular signaling in gut healthchronic inflammation and tissue damageepithelial cell fate regulationfibroblast lipid metabolismgut cell ferroptosisinflammatory bowel disease mechanismsiron-dependent cell deathlipid peroxidation in inflammationmetabolic dynamics in intestinal fibroblastsreactive oxygen species in IBDtargeted therapeutic strategies for IBD