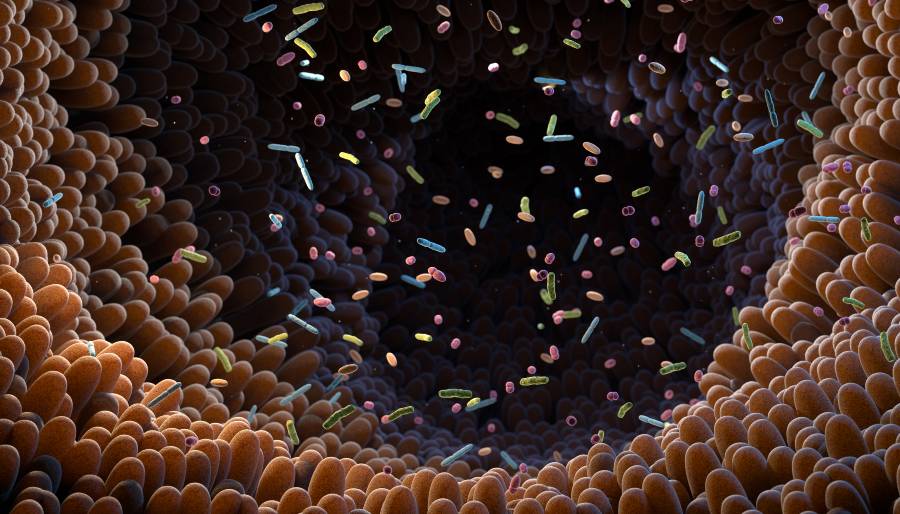
Trimethylamine (TMA), a molecule produced from dietary choline by gut bacteria, has been shown to block a key immune pathway and improve blood sugar control. This microbial molecule may provide a surprising boost in the fight against insulin resistance and type 2 diabetes.
“This shows how nutrition and our gut microbes can work together by producing molecules that fight inflammation and improve metabolic health,” said Patrice Cani, PhD, professor of Physiology, Metabolism and Nutrition at the Louvain Drug Research Institute (LDRI) of the University of Louvain, Belgium and visiting professor at Imperial College London.
This work appears in Nature Metabolism in the paper, “Inhibition of IRAK4 by microbial trimethylamine blunts metabolic inflammation and ameliorates glycemic control.”
Two decades ago, Cani discovered that a high-fat diet leads to the presence of bacterial components in the body, which activates the immune system and triggers inflammation, eventually causing insulin resistance in diabetic individuals.
Now, a collaborative team has uncovered how to counter this process. They observed that TMA, produced by gut bacteria from the natural nutrient choline—which is found in certain foods—can improve blood-sugar control.
TMA does this by acting as a natural inhibitor of the IRAK4 protein—a key component of the immune system. Normally, when exposed to a high-fat diet, IRAK4 triggers inflammation to signal dietary imbalance. With constant overload (as seen in type 2 diabetes), IRAK4 overreacts, causing cascading inflammation that drives insulin resistance.
By combining human cell models, mouse studies, and molecular-target screening, the team discovered that TMA can bind directly to IRAK4 and block its activity. The direct effect is a reduction in fat-induced inflammation and a restoration of insulin sensitivity. In essence, it reprograms the negative metabolic responses caused by poor diet. Even more striking: the molecule can prevent sepsis-induced mortality in mice by blocking widespread inflammation.
The team also observed that genetically deleting IRAK4 or blocking it pharmacologically reproduced the beneficial effects of the bacterial metabolite. This opens new therapeutic avenues for diabetes, using the target IRAK4, that is already validated within the pharmaceutical industry.
“This flips the narrative,” said Marc-Emmanuel Dumas, PhD, chair in Systems Medicine and head of the Division of Systems Medicine in the Department of Metabolism, Digestion and Reproduction at Imperial College London & CNRS. “We’ve shown that a molecule from our gut microbes can actually protect against the harmful effects of a poor diet through a new mechanism. It’s a new way of thinking about how the microbiome influences our health.”
With more than 500 million people worldwide affected by diabetes, identifying TMA as a microbial signal that modulates immunity could pave the way for new treatments. Nutritional strategies or drugs designed to boost TMA production may offer a new approach to combating insulin resistance and its complications.