Cardiovascular disease is the leading cause of death worldwide and often originates in atherosclerosis, a chronic condition in which inflammation and fat deposits cause arteries to harden and narrow. Although clinical practice already targets causal factors like cholesterol, hypertension, and smoking, detecting atherosclerosis in its early stages remains challenging.
A study in mice and in humans, led by researchers at Centro Nacional de Investigaciones Cardiovasculares (CNIC), has now identified a gut microbiota–derived metabolite, imidazole propionate (ImP), that appears in the blood during the early stages of active atherosclerosis.
“This metabolite is uniquely produced by intestinal bacteria,” explains CNIC researcher Annalaura Mastrangelo, PhD, one of the study’s two first authors. The team found that ImP was highly associated with atherosclerosis in an atherosclerosis-prone mouse model, when animals were fed high-cholesterol (HC) diets. They also found that ImP was associated with the extent of atherosclerosis in two independent human cohorts, including asymptomatic volunteers either with, or without subclinical atherosclerosis. “Our study shows that its presence in the bloodstream is associated with the development of active atherosclerosis in people who otherwise appear healthy,” Mastrangelo continued.
Findings from the human cohorts, the team continued, “… reveal a strong association between ImP and atherosclerosis, particularly active atherosclerosis, suggesting its potential use as an indicator of early active atherosclerosis before other comorbidities become confounding factors.”
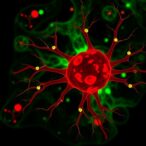
![Aortas from mice treated with the bacterial metabolite imidazole propionate (ImP) and a drug that blocks its pro-atherogenic effect. Atherosclerotic plaques are stained red. Bottom: Aortas from mice fed a high-cholesterol diet to induce atherosclerosis over eight weeks and treated with the ImP-blocking drug during the final four weeks. Atherosclerotic plaques are stained red. [CNIC]](https://www.genengnews.com/wp-content/uploads/2025/07/low-res-2-217x300.jpeg)
In their paper, reported in Nature (“Imidazole propionate is a driver and therapeutic target in atherosclerosis”) the investigators noted that previous studies have focused on associations of ImP and other microbiota-dependent metabolites with advanced stages of CVD or mortality. “Specifically, ImP has been related to type II diabetes, cardiometabolic disease in people with HIV, coronary artery disease and heart failure.”
Mastrangelo emphasizes that the new discovery has important clinical implications. “Detecting this blood marker offers a major advantage because current diagnostic tools rely on advanced imaging techniques that are complex, expensive, and not covered by public health systems. Blood levels of ImP provide a diagnostic marker that could help identify apparently healthy individuals with active atherosclerosis, and thus enable earlier treatment.”
Through their research the team also found that administering ImP to atherosclerosis-prone mice fed a normal diet was enough to induce atherosclerosis without altering the lipid profile, and this was linked to activation of systemic and local innate and adaptive immunity and inflammation. In the mouse models, they stated, “… ImP supplementation increased atherosclerosis development in the aorta and aortic root without affecting circulating cholesterol or glucose concentration.”
Further analyses showed that animals treated with ImP for eight weeks demonstrated relative increases in the numbers of fibroblasts, endothelial cells and immune cells in the aorta. The animal data, the investigators noted, “… identify ImP as a novel contributor to atherosclerosis etiology in atherosclerosis-prone mice that is associated with activation of the immune response without affecting the bloodstream concentration of cholesterol.”
Co–first author Iñaki Robles-Vera, PhD, further explained. “We not only observed elevated ImP levels in people with atherosclerosis, but also showed that ImP itself is a causal agent of the disease.” In animal models of atherosclerosis, Robles-Vera noted, ImP administration led to the formation of arterial plaques. It does this by activating the imidazoline receptor type 1 (I1R), which increases systemic inflammation and promotes atherosclerosis development. “Specifically, we found that ImP caused atherosclerosis through the imidazoline-1 receptor (I1R, also known as nischarin) in myeloid cells,” the team stated.
Through their newly reported research the scientists showed that blocking the I1R receptor prevents ImP-induced atherosclerosis and slowed disease progression in mouse models fed a high-cholesterol diet. David Sancho, PhD, head of the CNIC Immunobiology Laboratory and lead author on the study, said the discovery is important because it could open the way to a completely new line of treatment.
“This suggests that future treatment could combine I1R blockade with cholesterol-lowering drugs to produce a synergistic effect that prevents atherosclerosis development,” explained Sancho. “These findings open new possibilities for the early detection and personalized treatment of atherosclerosis,” he continued. “Instead of focusing solely on cholesterol and other classic risk factors, we may soon be able to analyze blood for ImP as an early warning signal. At the CNIC, we are also working to develop drugs that block the detrimental effects of ImP.”
In their paper the researchers pointed out that while lipid-lowering therapy is currently used to prevent atherosclerosis progression, the rate of cardiovascular events remains high even in patients receiving appropriate lipid-lowering treatments. “… we propose the ImP–I1R axis in myeloid cells as an independent target for atherosclerosis therapy that may potentially synergize with current treatments.”