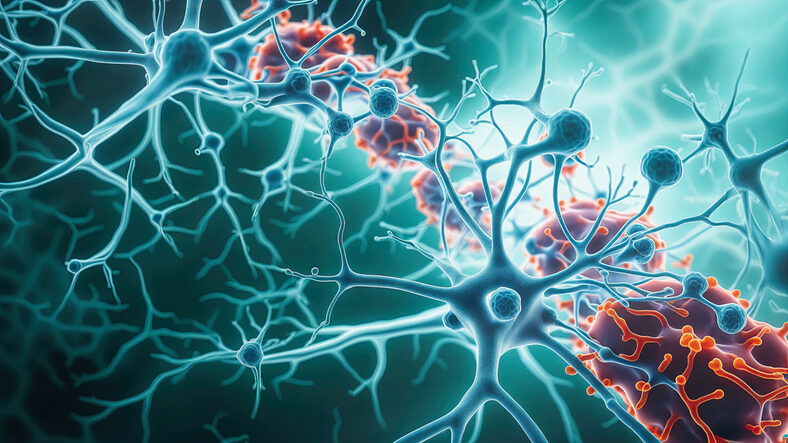
Parkinson’s disease (PD) is defined by the progressive loss of dopaminergic neurons in the substantia nigra, but the biological forces that push these neurons toward degeneration remain only partly understood. Microglia—the brain’s resident immune cells—have long been implicated in this process. They become reactive early in disease, cluster around vulnerable neurons, and release inflammatory factors. Yet the precise trigger that converts microglia from protective sentinels into active participants in neuronal destruction has remained elusive.
A new study published in npj Parkinson’s Disease, “Microglial low-affinity FcγR mediates the phagocytic elimination of dopaminergic neurons in Parkinson’s disease degeneration,” offers a mechanistic explanation. Researchers at the Institut de Neurociències of the Universitat Autònoma de Barcelona (INc‑UAB) and the UAB department of biochemistry and molecular biology report that microglia in PD appear to eliminate dopaminergic neurons through an Fc gamma receptor (FcγR)–driven phagocytic program—and that blocking this receptor with immunotherapy can prevent neuron loss in disease models.
The team began by examining postmortem brain tissue from PD patients. As expected, the substantia nigra contained a high proportion of reactive microglia, consistent with chronic neuroinflammation. But a more striking finding emerged: these reactive microglia expressed elevated levels of low‑affinity Fcγ receptors (CD16 and CD32). These receptors normally help immune cells identify damaged or antibody‑tagged targets for clearance. In PD, however, the researchers propose that FcγRs may be misidentifying still‑viable dopaminergic neurons as debris.
This pattern was mirrored in the MPTP mouse model of PD, where microglia also upregulated FcγRs and physically engaged degenerating dopaminergic neurons. Prior work from the same group had shown that microglia make direct body‑to‑body contact with vulnerable neurons before their disappearance, suggesting an active phagocytic process rather than passive degeneration.
To test whether FcγRs were driving this elimination, the researchers turned to both in vitro and in vivo systems. In co‑cultures modeling an interferon‑γ–driven inflammatory environment, microglia readily engulfed dopaminergic cells—but this phagocytosis was sharply reduced when FcγRs were blocked with neutralizing antibodies. In parallel, inhibiting Cdc42, a cytoskeletal regulator downstream of FcγR signaling, also prevented microglia from forming the actin‑rich “phagocytic cup” required to engulf neurons.
“Finally, passive immunotherapy using CD16/32 neutralizing monoclonal antibodies in MPTP-treated mice protected DA neurons from elimination, suggesting a novel and viable potential therapeutic strategy for PD,” the authors wrote. This intervention preserved dopaminergic neurons even under conditions of intense neuroinflammation.
“What is particularly interesting is that in animal and cellular models of the disease, blocking Fc gamma receptors with immunotherapy, as well as pharmacologically inhibiting Cdc42, significantly reduced the elimination of dopaminergic neurons, preserving them even under conditions of intense neuroinflammation,” said corresponding author Carlos Barcia, PhD, from UAB.
Together, the findings position FcγR‑mediated phagocytosis as a central mechanism of dopaminergic neuron loss in PD—and highlight microglial FcγR as a promising immunotherapeutic target. While the work remains preclinical, it opens a new translational path: instead of trying to rescue neurons after they degenerate, future therapies might prevent microglia from mistakenly “eating” them in the first place.