Because of its pivotal role in cell cycle regulation—and its overexpression in various types of cancer—membrane-associated tyrosine-threonine protein kinase 1 (PKMYT1) has emerged as a promising therapeutic target in oncology. Past research has shown that inhibiting PKMYT1 via synthetic lethality enables the enzyme to selectively eliminate cancer cells bearing specific genetic mutations such as FBXW7 and PPP2R1A, or CCNE1 amplification, while sparing normal healthy cells and minimizing adverse effects.
Applying those insights, a team of researchers at Insilico Medicine has used the company’s Chemistry42 generative artificial intelligence (AI) platform to design a first-in-class proteolysis-targeting chimera (PROTAC) designed to target PKMYT1, also known as Myt1 kinase.

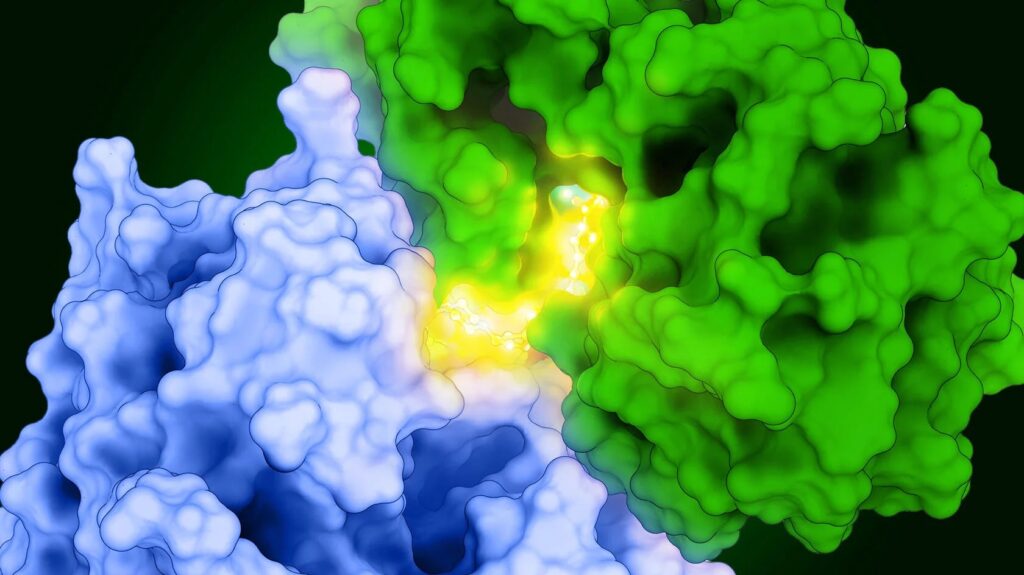
In “Discovery of a bifunctional PKMYT1-targeting PROTAC empowered by AI-generation,” a paper published in Nature Communications, Insilico researchers detailed their creation of their preclinical lead PROTAC, a bifunctional PKMYT1 degrader called D16-M1P2, by linking a novel PKMYT1 inhibitor to an optimized binder of the protein cereblon (CRBN).
Insilico has not announced any specific priority indications for the PROTAC. In preclinical studies, D16-M1P2 showed consistent potency in CCNE1-amplified breast cancer cell lines and in an FBXW7-mutant cholangiocarcinoma (bile duct cancer) line, as well as in a CCNE1-amplified breast cancer xenograft model.
“Those data suggest that CCNE1-amplified and FBXW7/PPP2R1A-altered tumors, including subsets of breast, bile duct, and other solid cancers, could be particularly well suited for this mechanism,” Alex Zhavoronkov, PhD, the paper’s corresponding author and Insilico’s founder, chairman, executive director, and CEO, told GEN. “The biology in the paper points us toward tumors that harbor specific genomic alterations rather than a single histology.”
The studies reflect the fact PKMYT1 dependency is strongest in cells with CCNE1 amplification or loss-of-function alterations in FBXW7 or PPP2R1A, which occur across several solid tumor types.
“Any future clinical development plan would be expected to focus on patients whose tumors carry these biomarker profiles, guided by the synthetic lethality and dependency signals we describe in the paper,” he added.
‘Promising lead’
D16 is a mixture of stereoisomers that share the same overall architecture, PKMYT1 warhead, linker, and CRBN ligand, but differ in their three-dimensional arrangement. When researchers separated D16 into individual stereoisomers, D16-M1P2 emerged as the configuration that formed the most productive ternary complex with PKMYT1 and CRBN.
That stereochemistry, Insilico reasons, leads to more efficient PKMYT1 degradation at lower concentrations and stronger downstream inhibition of CDK1 phosphorylation. D16-M1P2 takes the same basic design and “locks” it into the 3D shape that best supports ubiquitination and degradation, which in turn improves functional pathway inhibition without changing the basic components of the PROTAC.
The researchers reported that D16-M1P2 showed dual mechanisms of PKMYT1 degradation and inhibition, with strong antiproliferative potency facilitated by high selectivity. D16-M1P2 also showed favorable oral bioavailability, stronger pharmacodynamic effects than those of the PKMYT1 inhibitor alone, and robust antitumor response as a monotherapy in xenograft models.
“This PROTAC serves as a precise chemical probe to explore PKMYT1 biology and a promising lead for further cancer therapy exploration,” the Insilico researchers concluded.
PROTAC development has progressed since 2019, when Arvinas advanced the first PROTAC into the clinic, ARV-110 (now called bavdegalutamide), which targets the androgen receptor (AR) and is designed to treat metastatic castration resistant prostate cancer (mCRPC). While ARV-110 showed anti-tumor activity and a favorable safety profile in a Phase I/II trial (NCT03888612), Arvinas ended the program and pivoted to a next-generation version, ARV-766 (vepdegestrant), which it agreed to co-develop through an up-to-$1.161 billion ($150 million upfront) collaboration with Novartis in 2024.
In April, however, Arvinas researchers published positive preclinical data for bavdegalutamide: “These data suggest that bavdegalutamide could have efficacy as a later-line mCRPC treatment for patients who have developed resistance to the ARPIs that are currently the standard of care for mCRPC.”
The number of PROTAC molecules has zoomed from a few dozen bifunctional degraders in 2015 to more than 6,000 listed in public repositories spanning hundreds of E3 ligases and warheads, Riyaz Syed, PhD, founder and CEO of Centella AI Therapeutics, reported October 29 in a blog post shared on Medium. Thanks to public resources like PROTACpedia and PROTAC-DB 3.0, Syed wrote, “AI has become the silent catalyst transforming targeted protein degradation.”
‘Data-driven era’
“From DeLinker to PROTAC-RL, and from PROTAC-DB 3.0 to AlphaFold-Multimer, PROTAC design is entering a data-driven era were learning complements human intuition,” he observed.
Most AI-PROTAC work, Zhavoronkov said, “so far has focused on using AI to decorate an existing warhead with a linker and an E3 ligand.
“In our case, AI was used end-to-end,” he added.
Zhavoronkov said Insilico used AI to first invent a completely new PKMYT1 inhibitor chemotype, then design and optimize the PROTAC itself. Using Chemistry42, Insilico researchers combined structural information from a clinical PKMYT1 inhibitor and another kinase inhibitor known to bind PKMYT1.
The team generated more than 2,000 novel molecules, and iteratively optimized them for potency, kinome selectivity, and ADMET (absorption, distribution, metabolism, excretion, and toxicity) to arrive at a new scaffold extending from deep within the PKMYT1 target binding pocket out to the solvent front area, creating a built-in attachment point for PROTAC design.
“We then used structure-based modeling of the PKMYT1–E3 ternary complex and generative linker design to optimize the bifunctional molecule for degradation efficiency and drug-like PK,” Zhavoronkov explained. “D16-M1P therefore is not just an ‘AI-decorated’ version of an existing drug, but both the warhead and the PROTAC are AI-generated and jointly optimized, giving us a highly selective PKMYT1 degrader/inhibitor with potent pathway inhibition, durable target engagement, and favorable oral exposure in preclinical models.”
Anti-tumor qualities
Three qualities enable D16-M1P2 to achieve potent anti-tumor activity with high selectivity and favorable oral bioavailability, Insilico said, starting with selectivity. D16-M1P2 uses an AI-generated “warhead” designed to be highly selective at the kinase level. Testing in a 400+ kinase panel demonstrated D16-M1P2 to show strong preference for PKMYT1 over other kinases, an outcome the researchers said helps minimize off-target liabilities that often limit dose.
In the kinase panel test, Zhavoronkov said, D16-M1P2 showed over 50-fold selectivity for PKMYT1 over the next-highest binding off-target kinases compared to Repare Therapeutics’ lunresertib (RP-6306)—the first PKMYT1 inhibitor to enter clinical trials—which had ~10-fold selectivity for PKMYT1 over BRAF, RAF1, and SRC, and over 10 times as many significant off-target hits.
D16-M1P2 also showed:
- Dual mechanism: At lower concentrations, D16-M1P2 degraded PKMYT1 via CRBN and the ubiquitin–proteasome system, while at higher concentrations, the PROTAC acted as a reversible kinase inhibitor, enabling PKMYT1 signaling to be suppressed across a broad exposure range.
- Drug-like PK: D16-M1P2 uses an AI-guided linker and E3-ligand optimization to improve solubility, free fraction, and permeability while maintaining degradation efficiency, a feature Insilico says translated into good oral bioavailability and sustained tumor target engagement in xenograft models.
“This combination of selectivity, dual mechanism, and drug-like PK achieved the potent, biomarker-linked antitumor activity described,” Zhavoronkov said.
Among the challenges researchers faced and surmounted, he said, were designing a warhead that maintained strong PKMYT1 binding but dramatically reduced off-target kinase activity. Insilico’s AI models helped researchers explore novel hinge-binding motifs and substituents that preserved key PKMYT1 interactions while disfavoring binding to closely related kinases. “That yielded a new scaffold with high biochemical potency, a very clean kinome profile, and a primary amine ‘handle’ positioned optimally for linker attachment.”
On the PROTAC side, Zhavoronkov continued, the main challenges were achieving efficient ternary complex formation and degradation without sacrificing basic drug-like properties. While flexible linkers offer degradation, they often lead to poor permeability, high efflux, and low oral exposure. Using structure-based modeling of the PKMYT1–E3 ternary complex together with Chemistry42, the Insilico researchers systematically varied CRBN binders and linkers, introducing rigid, spirocyclic elements and tuning linker length and polarity.
“This produced D16 and ultimately the single stereoisomer D16-M1P2, which combines potent degradation and target inhibition with improved solubility, permeability, and oral PK. This combination is hard to reach with a traditional trial-and-error PROTAC linker design,” Zhavoronkov said.
Chemistry42 is Insilico’s drug discovery engine used for designing and optimizing novel small molecule drug candidates with desired properties from scratch, by using various AI models to streamline hit identification, hit-to-lead, and lead optimization.
Degrading and inhibiting
Why does PKMYT1 require both degrading and inhibiting?
The paper offered a reason: Even when PKMYT1 protein levels are reduced by 80–90%, some CDK1 phosphorylation and signaling persisted, suggesting that degradation alone may not fully shut down the Wnt signaling pathway. Researchers also found that degradation contributed to more sustained downstream signal inhibition, with pCDK1 ablated for at least 24 hours after D16-M1P2 treatment and washout, while PKMYT1 inhibition alone resulted in inhibition that bounced back after only two hours.
To design a molecule that is both a degrader and an inhibitor, Zhavoronkov said, Insilico researchers addressed both aspects of PKMYT1 biology. At lower exposures the PROTAC component is designed to efficiently remove PKMYT1 protein, allowing for meaningful target suppression at doses where a purely inhibitory agent might struggle, potentially creating room for a better safety margin. At higher exposures, the built-in kinase inhibitor continues to block PKMYT1’s catalytic activity even as degradation begins to plateau.
“Rather than choosing between degrade or inhibit, our data supports a dual-mechanism strategy that can provide deeper and more durable pathway inhibition while relying on a more selective chemical scaffold than first-generation PKMYT1 inhibitors,” Zhavoronkov said.
However, any safety advantages will require confirmation in future preclinical and clinical studies, he added.
Insilico’s next steps are to complete pre-candidate work, understand the safety and efficacy window in more depth, and decide whether to nominate D16-M1P2 or a related analog as a candidate for clinical development.
“D16-M1P2 has shown a compelling profile as a chemical probe and lead in preclinical experiments, and is undergoing more extensive characterization, including additional PK/PD work, safety and tolerability studies, and broader efficacy assessment, to determine whether it merits progression into full development as a clinical candidate,” Zhavoronkov said.