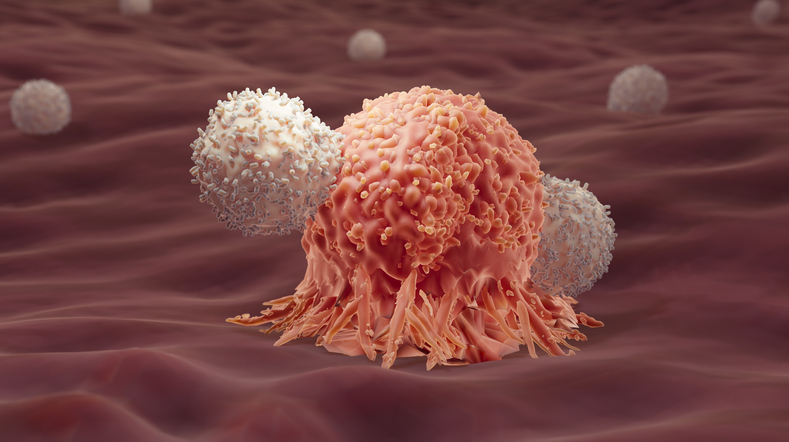
Cancer immunotherapy seeks to harness the natural protective ability of our immune system to fight against cancer. A market report published by Grand View Research estimated that the global cancer immunotherapy market size is expected to grow from a current value of $125.7 billion with a compound annual growth rate (CAGR) of 8.3% from 2025 to 2030. The FDA is also expected to approve more cancer immunotherapies over the next five years.
In the last two years, several startups have also raised significant funds to develop their cancer immunotherapies, including Bicara Therapeutics’ $108 million Series B financing round and Domain Therapeutics’ $42 million Series A round.
GEN recently spoke to Qi Zeng, PhD, founder and CSO of Intra-ImmuSG (IISG), a Singapore-based clinical-stage spinoff biotechnology company from the Agency for Science, Technology & Research (A*STAR), on their unconventional approach to targeting intracellular oncoproteins with antibodies and how this strategy has enabled them to recently complete a successful Phase II clinical trial.
GEN: What challenges are IISG trying to overcome in the field of cancer therapy?
Zeng: There are several challenges in cancer therapy that IISG is tackling. Most current immunotherapies target a limited number of extracellular proteins or receptors expressed in both cancer cells as well as normal cells involved in general immune regulation that are not tumor specific, resulting in undesirable immune-related side effects. In addition, only a fraction of cancer patients are responsive to current immunotherapy.
On the other hand, the most current targeted chemotherapies against tumor-specific intracellular oncotargets or mutated genes cause off-target side effects and drug resistance. Importantly, the overall cancer survival of most cancer types is still limited, with some experiencing high recurrence rates. Hence, there is an impetus to continue the search for tumor-specific targets and the development of novel targeted therapies to increase the efficacy of treatment.
In 1998, my team and I identified the PRL3 gene and its association with cancer (Zeng et al., 1998). In 2001, Bert Vogelstein, MD, from Johns Hopkins University, reported the association of PRL3 with cancer and cancer metastasis (Saha et al., 2001). Subsequent studies from many other labs globally have shown the involvement of PRL3 in diverse cancer types via its role in regulating various cancer signaling pathways associated with hallmarks of cancer (Chia et al., 2023).
My lab further demonstrated that 80.6% of tumor tissues overexpressed PRL3 proteins, but not in matched normal tissues (Thura et al., 2019). This makes PRL3 an excellent tumor-specific pan-cancer target that could potentially be used against multiple cancer types.

By convention, antibody drugs (immunotherapy) target extracellular oncoproteins, while small chemical compounds (chemotherapy) target intracellular oncoproteins, such as PRL3 intracellular oncoproteins. However, both immunotherapy and chemotherapy modalities are aimed at targets with suboptimal tumor specificity and are facing drug resistance over time. Based on our serendipitous research findings, we proposed using antibody drugs against intracellular oncoproteins as a novel cancer immunotherapy (Guo et al., 2011), which challenged the current immunotherapy dogma at that time.
My motivations are to develop a safer and more effective cancer therapy via a combination of a targeted therapy and immunotherapy that recruits host immune cells to tumor sites to kill cancer cells, thus enhancing safety and drug efficacy.
GEN: What are some ups and downs that IISG has faced over the last few years?
Zeng: Since 2008, my lab has published several research articles based on robust data using cancer mouse models to preclinically support the unconventional idea that a cancer immunotherapy antibody can block tumors that express externalized PRL3 oncoproteins (Guo et al., 2008; Guo et al., 2011; Guo et al., 2012; Thura et al., 2016; Thura et al., 2019; Thura et al., 2021). The detailed Mechanism of Action (MOA) of this approach was revealed in 2019 (Thura et al., 2019). Due to the stresses in the in vivo tumor microenvironment such as nutrient deprivation, hypoxia, and necrosis, some intracellular PRL3 proteins are externalized onto the cancer cell surface as extracellular PRL3 antigen via several mechanisms that include but are not limited to the exosomal secretion pathway. PRL3-zumab could thus bind to the “externalized PRL3 antigen” and trigger host anti-tumor immunity to significantly reduce tumor burdens and improve survival.
Due to the uniqueness and scientific robustness of the proposed immunotherapy, IISG successfully obtained multinational clinical trial approvals of PRL3-zumab from regulatory authorities. In 2020, Investigational New Drugs (IND) clinical Phase II approvals were successfully obtained from the FDA, China’s National Medical Products Administration (NMPA), and Malaysia’s National Pharmaceutical Regulatory Agency (NPRA) to perform multi-national Phase II clinical trials. In addition, IISG had also conducted a compassionate First-in-Child trial of PRL3-zumab in a 7-year-old male rhabdomyosarcoma patient at KK Women’s and Children’s Hospital Singapore. PRL3-zumab was shown to be safe in children, and it demonstrated clinical benefit in combination with radiotherapy (Loh et al., 2023).
Our recruited patients have benefited from PRL3-zumab treatment in extending life expectancy with a good life quality, and some patients with significantly reduced tumor burdens. An example of an advanced stage IV gastric cancer U.S.-based patient benefiting significantly from PRL3-zumab with an extension of progression-free-survival (PFS) and excellent quality of life despite the late stage is published in the public domain. Together, these trials have confirmed the excellent safety profile of PRL3-zumab in more than 200 advanced stage IV cancer patients and promising positive signals of drug efficacy in several aggressive cancer types in which these patients have few standard-of-care (SOC) treatment options.
GEN: What are the most recent developments you are excited about at IISG?
Zeng: With the excellent drug safety profile and clear positive signals of efficacy of PRL3-zumab, we are encouraged to push on into the next phase of clinical trials such as breakthrough trials for rare cancer types, and to investigate the potential of combination treatment with other approved therapies such as targeted cancer therapy or immunotherapy, as cancer is elusive and combination therapy is becoming an important approach in cancer therapy.
Our recent research has also demonstrated the intimate involvement of PRL3 with polyploid giant cancer cells that play a critical role in tumor relapse and PRL3-zumab was shown to prevent tumor relapse, opening the door for PRL3-zumab as an adjuvant therapy with surgery and radiotherapy to prevent tumor relapse. Among the patients who have benefitted from PRL3-zumab are several patients who have withdrawn from prior lines of immunotherapy due to toxicity or progressive disease. In these patients, PRL3-zumab exhibited more encouraging therapeutic effects with longer Progress Free Survival (PFS) than prior lines of treatment without drug-related toxicity. As such, IISG is excited about using PRL3-zumab for treating patients who are no longer suitable for immunotherapy (such as PD-1, PD-L1) or chemotherapy.
GEN: What message does IISG want to share with the community?
Zeng: Throughout seven years of clinical trials and in more than 200 cancer patients, PRL3-zumab has demonstrated high efficacy and safety profiles. This is exciting news for the continued clinical development of PRL3-zumab. Currently, we are actively seeking fundraising and partnership opportunities with biotech/pharmaceutical companies and venture capital funds to co-develop PRL3-zumab in these promising cancer indications via Phase IIb pivotal trials (confirmatory trials) and breakthrough pathways for drug approval to meet urgent unmet medical needs to benefit cancer patients in years to come.
Andy Tay, PhD, is a freelance science writer based in Singapore.
References:
Chia, P. L., Ang, K. H., Thura, M., & Zeng, Q. (2023). PRL3 as a therapeutic target for novel cancer immunotherapy in multiple cancer types [Review]. Theranostics, 13(6), 1876-1891. https://doi.org/10.7150/thno.79265
Guo, K., Li, J., Tang, J. P., Tan, C. P. B., Hong, C. W., Al-Aidaroos, A. Q. O., Varghese, L., Huang, C., & Zeng, Q. (2011). Targeting Intracellular Oncoproteins with Antibody Therapy or Vaccination. Science Translational Medicine, 3(99), 99ra85. https://doi.org/10.1126/scitranslmed.3002296
Guo, K., Tang, J. P., Li, J., Tan, C. P., Al-Aidaroos, A. Q. O., Hong, C. W., Varghese, L., Feng, Z. W., Park, J. E., Zhou, J. B., Chng, W. J., & Zeng, Q. (2012). Engineering the First Chimeric Antibody in Targeting Intracellular PRL-3 Oncoprotein for Cancer Therapy in Mice. Oncotarget; Vol 3, No 2: February 2012. https://www.oncotarget.com/article/442/text/
Guo, K., Tang, J. P., Tan, C. P., Wang, H., & Zeng, Q. (2008). Monoclonal antibodies target intracellular PRL phosphatases to inhibit cancer metastases in mice. Cancer Biol Ther, 7(5), 750-757. https://doi.org/10.4161/cbt.7.5.5764
Loh, A. H. P., Thura, M., Gupta, A., Tan, S. H., Kuan, K. K. Y., Ang, K. H., Merchant, K., Chang, K. T. E., Yon, H. Y., Chen, Y., Cheng, M. H. W., Mahadev, A., Ng, M. C. H., Seng, M. S., Iyer, P., Chia, P. L., Soh, S. Y., & Zeng, Q. (2023). Exploiting frequent and specific expression of PRL3 in pediatric solid tumors for first-in-child use of PRL3-zumab humanized antibody. Mol Ther Oncolytics, 30, 153-166. https://doi.org/10.1016/j.omto.2023.08.006
Saha, S., Bardelli, A., Buckhaults, P., Velculescu, V. E., Rago, C., St Croix, B., Romans, K. E., Choti, M. A., Lengauer, C., Kinzler, K. W., & Vogelstein, B. (2001). A phosphatase associated with metastasis of colorectal cancer. Science, 294(5545), 1343-1346. https://doi.org/10.1126/science.1065817
Thura, M., Al-Aidaroos, A. Q., Gupta, A., Chee, C. E., Lee, S. C., Hui, K. M., Li, J., Guan, Y. K., Yong, W. P., So, J., Chng, W. J., Ng, C. H., Zhou, J., Wang, L. Z., Yuen, J. S. P., Ho, H. S. S., Yi, S. M., Chiong, E., Choo, S. P., . . . Zeng, Q. (2019). PRL3-zumab as an immunotherapy to inhibit tumors expressing PRL3 oncoprotein. Nature Communications, 10(1), 2484. https://doi.org/10.1038/s41467-019-10127-x
Thura, M., Al-Aidaroos, A. Q. O., Yong, W. P., Kono, K., Gupta, A., Lin, Y. B., Mimura, K., Thiery, J. P., Goh, B. C., Tan, P., Soo, R., Hong, C. W., Wang, L., Lin, S. J., Chen, E., Rha, S. Y., Chung, H. C., Li, J., Nandi, S., . . . Zeng, Q. (2016). PRL3-zumab, a first-in-class humanized antibody for cancer therapy. JCI Insight, 1(9). https://doi.org/10.1172/jci.insight.87607
Thura, M., Ye, Z., Al-Aidaroos, A. Q., Xiong, Q., Ong, J. Y., Gupta, A., Li, J., Guo, K., Ang, K. H., & Zeng, Q. (2021). PRL3 induces polypoid giant cancer cells eliminated by PRL3-zumab to reduce tumor relapse. Commun Biol, 4(1), 923. https://doi.org/10.1038/s42003-021-02449-8
Zeng, Q., Hong, W., & Tan, Y. H. (1998). Mouse PRL-2 and PRL-3, two potentially prenylated protein tyrosine phosphatases homologous to PRL-1. Biochem Biophys Res Commun, 244(2), 421-427. https://doi.org/10.1006/bbrc.1998.8291