In a groundbreaking study poised to reshape our understanding of Alzheimer’s disease, researchers have uncovered compelling evidence pointing to the intracellular buildup of amyloid-beta (Aβ) as a critical marker of selective neuronal vulnerability. This discovery, recently published in Nature Communications, elucidates a previously underappreciated layer of complexity in the pathogenesis of Alzheimer’s, one of the most devastating neurodegenerative disorders affecting millions worldwide. The study’s findings may pivot future therapeutic strategies towards targeting neuronal compartments previously overlooked in the fight against cognitive decline.
Alzheimer’s disease (AD) has long been associated with extracellular amyloid plaques and neurofibrillary tangles composed of tau protein. Traditional models have emphasized amyloid-beta’s extracellular aggregation as a primary driver of neurotoxicity and synaptic dysfunction. However, these perspectives have failed to fully account for why specific neuronal populations succumb earlier than others, a phenomenon known as selective neuronal vulnerability. The current research confronts this paradox by focusing on the intracellular accumulation of amyloid-beta peptides, unveiling a crucial intracellular pathological feature.
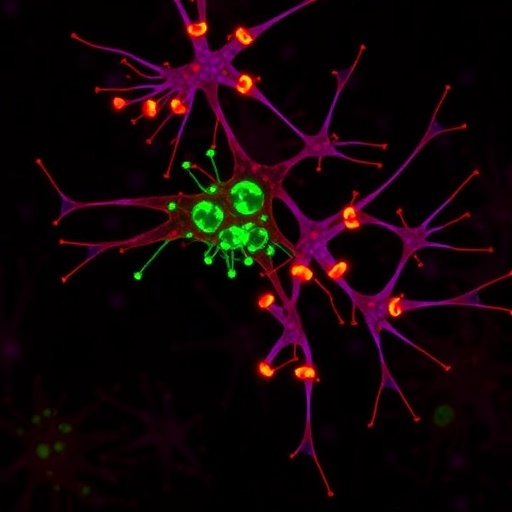
The team behind the study, led by Anna Caramello, Nicolas Fancy, and Cyril Tournerie, employed state-of-the-art imaging techniques combined with advanced biochemical analyses to meticulously map the distribution and localization of amyloid-beta within neurons derived from human and animal models of Alzheimer’s disease. Their approach allowed for subcellular resolution of amyloid-beta accumulation, unmasking the intracellular compartments where pathological build-up preferentially occurs. This precision revealed a stark contrast between vulnerable and resistant neuronal subtypes.
.adsslot_Ku7XJwtEDk{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_Ku7XJwtEDk{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_Ku7XJwtEDk{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Intracellular amyloid-beta was found to accumulate predominantly in the soma and proximal dendrites of vulnerable neurons, regions essential for maintaining neuronal health and signaling. The accumulation correlated strongly with markers of cellular stress and synaptic dysfunction, implicating intracellular Aβ not just as a byproduct, but as a possible instigator of neurodegenerative cascades. This observation challenges the long-standing dogma narrowly attributing toxicity to extracellular plaques alone, suggesting that neurodegeneration likely initiates within the neuron before propagating outward.
Importantly, the researchers demonstrated that intracellular amyloid-beta accumulation precedes overt signs of neuronal death, indicative of its role as an early marker rather than a nonspecific consequence of advanced pathology. By exploring various stages of AD progression in postmortem brains and experimental models, they charted a temporal trajectory where intracellular pockets of amyloid-beta begin to exert toxic effects, disrupting cellular machinery and triggering apoptotic pathways, ultimately leading to selective neuronal loss.
The molecular mechanisms underpinning this intracellular accumulation were also probed. The study highlighted disruptions in the endosomal-lysosomal and autophagy pathways, cellular processes responsible for protein degradation and recycling. Faulty clearance of amyloid-beta within these systems appears to facilitate its build-up, supporting a model whereby intracellular proteostasis failure contributes to disease progression. Such insights open avenues for therapeutic interventions aimed at restoring these degradative functions.
Further fascinating was the discovery of neuron-type specificity in amyloid-beta accumulation. Vulnerable populations—such as entorhinal cortex layer II pyramidal neurons and certain hippocampal subfield neurons—exhibited markedly higher intracellular Aβ levels compared to resistant neuronal populations. This selectivity provides a molecular rationale for the pattern of neurodegeneration observed clinically, linking intracellular amyloid pathology to cognitive decline patterns characteristic of early Alzheimer’s disease.
These revelations carry substantial implications for biomarker development. Intracellular amyloid-beta could serve as a more sensitive and earlier indicator of neuronal dysfunction compared to extracellular plaque burden measured by current imaging modalities. Efforts to detect intracellular amyloid-beta through cerebrospinal fluid sampling or advanced PET tracers could revolutionize diagnostic precision, enabling earlier intervention and monitoring of therapeutic efficacy.
Therapeutically, the results advise a shift from an exclusive focus on extracellular amyloid clearance to strategies that address intracellular amyloid-beta dynamics. Modulating intracellular trafficking, enhancing autophagy, and fortifying lysosomal functions emerge as promising targets. Such approaches may mitigate the early neuronal dysfunction that triggers downstream pathological cascades, potentially arresting or delaying disease onset.
Moreover, this study sheds light on why many clinical trials targeting extracellular amyloid-beta have failed to produce meaningful cognitive benefits. It suggests that insufficient attention to intracellular pools might underlie therapeutic resistance, emphasizing the need for a more holistic view of amyloid pathology. Future clinical trial designs may benefit from incorporating agents capable of penetrating neurons and modulating intracellular amyloid levels.
The methodological advances enabling this study are themselves notable. The integration of high-resolution fluorescence microscopy, immunogold labeling, and quantitative proteomics set a new standard for investigating subcellular amyloid distributions. These technical triumphs not only enhance the fidelity of molecular pathology studies but also inspire cross-disciplinary applications in neurodegenerative research more broadly.
In conclusion, the identification of intracellular amyloid-beta as a biomarker of selective neuronal vulnerability reframes the Alzheimer’s disease narrative. It beckons researchers and clinicians alike to reconsider the intracellular landscape as a battleground where the earliest and most consequential pathogenic events unfold. This nuanced understanding enriches our synopsis of disease mechanisms and offers a hopeful horizon for innovative diagnostic and therapeutic strategies aimed at preserving the intricate networks sustaining cognition.
As the global population ages, the urgency to unravel Alzheimer’s intricacies intensifies. Studies such as this underscore the vitality of basic and translational neuroscience synergy. By embracing the complexity of intracellular amyloid-beta dynamics and their neuronal specificity, the scientific community moves closer to unmasking the enigmatic origins of Alzheimer’s and designing interventions that might one day stave off its relentless advance.
Subject of Research: Intracellular accumulation of amyloid-beta as a marker for selective neuronal vulnerability in Alzheimer’s disease.
Article Title: Intracellular accumulation of amyloid-ß is a marker of selective neuronal vulnerability in Alzheimer’s disease.
Article References:
Caramello, A., Fancy, N., Tournerie, C. et al. Intracellular accumulation of amyloid-ß is a marker of selective neuronal vulnerability in Alzheimer’s disease. Nat Commun 16, 5189 (2025). https://doi.org/10.1038/s41467-025-60328-w
Image Credits: AI Generated
Tags: amyloid plaques and neurofibrillary tanglesamyloid-beta and synaptic dysfunctionbiochemical analysis of amyloid-betaimaging techniques in neuroscienceintracellular amyloid-beta accumulationNature Communications study on Alzheimer’sneurodegenerative disorders researchneuronal compartments in cognitive declinepathological features of Alzheimer’s diseaseselective neuronal vulnerability in Alzheimer’stherapeutic strategies for Alzheimer’s diseaseunderstanding Alzheimer’s disease mechanisms