In a groundbreaking clinical trial published recently in Nature Communications, researchers have unveiled compelling evidence showcasing the safety and efficacy of levamisole regimens in treating loiasis—a parasitic infection that has long challenged medical professionals in endemic regions. This double-blind, randomized, placebo-controlled study is one of the most comprehensive assessments to date, meticulously comparing the therapeutic outcomes of 3-day and 5-day levamisole courses. The findings prompt a re-evaluation of current treatment paradigms for loiasis and potentially pave the way for more accessible and effective interventions against this neglected tropical disease.
Loiasis, caused by the filarial nematode Loa loa, is transmitted to humans through the bite of infected deer flies (Chrysops species). The disease is characterized by the migration of adult worms through subcutaneous tissue and occasionally across the conjunctiva of the eye, causing discomfort and eye irritation. Beyond these hallmark symptoms, loiasis can induce serious complications, including neurological manifestations and kidney problems. Despite its significant health burden, options for effective and safe treatment have remained limited, primarily due to the potential severe adverse reactions elicited by existing medications in patients with high microfilarial loads.
Levamisole, a broad-spectrum antihelminthic and immunomodulatory agent, has been in clinical use for decades mainly in parasitic infections such as ascariasis and strongyloidiasis. However, its role in the treatment of loiasis has been comparatively underexplored, especially given concerns about tolerability and efficacy. In the present study, the research team sought to fill this critical knowledge gap by rigorously evaluating short-course levamisole treatments under tightly controlled conditions, ensuring that results not only demonstrate effectiveness but also guarantee patient safety.
.adsslot_1EpBKh3kSN{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_1EpBKh3kSN{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_1EpBKh3kSN{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
The trial enrolled a substantial cohort of patients diagnosed with loiasis from endemic regions, carefully stratified to balance age, sex, and baseline microfilarial density. Participants were randomly assigned to receive either a placebo, a 3-day levamisole regimen, or a 5-day regimen, with neither patients nor researchers aware of group assignments to minimize bias. The design underscored scientific rigor, heightening confidence in observed outcomes and their potential applicability to broader populations in endemic zones.
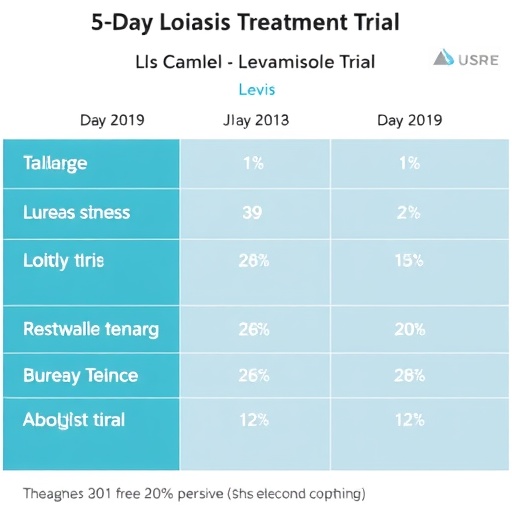
Upon completion of treatment, patients were monitored extensively over a prolonged period to assess reductions in microfilarial load and to detect any adverse events. The results were striking. Both levamisole regimens demonstrated a significant decrease in circulating microfilariae compared to placebo, with the 5-day treatment showing a more pronounced and sustained effect. Importantly, safety profiles were acceptable across both treatment arms, with only mild and transient side effects reported, suggesting that short-course levamisole therapy could circumvent previous concerns about drug-induced complications in loiasis patients.
One of the critical insights emerging from the study is the potential immunomodulatory role of levamisole in modulating host responses to filarial infection. Beyond its direct anthelmintic action, levamisole may enhance host immune defenses, facilitating clearance of microfilariae. This dual mechanism could explain the observed efficacy, especially notable given the historical difficulty in reducing microfilarial burden without triggering severe inflammatory reactions. Future research may delve deeper into these immunological pathways to optimize therapeutic protocols further.
This study also holds profound implications for public health strategies aimed at controlling loiasis in endemic areas. Current standard treatments, such as diethylcarbamazine and ivermectin, can provoke life-threatening encephalopathies in patients harboring high microfilarial densities—a significant barrier to mass drug administration campaigns. Safe alternatives like optimized levamisole regimens could transform the landscape of loiasis control, enabling more widespread and safer interventions, reducing disease incidence, and mitigating associated morbidity.
Of particular note is the randomized, placebo-controlled, and double-blind design of this trial, considered the gold standard in clinical research. Such methodological rigor eliminates many confounders, lending robust credibility to the findings. Moreover, the multicenter nature of the trial, spanning diverse populations within endemic regions, enhances the generalizability of results—critical for global health stakeholders considering deployment of this treatment in varied epidemiological contexts.
Beyond the immediate scope of loiasis, these findings may ripple across the broader field of neglected tropical diseases. The success of levamisole as a safe, short-course anthelmintic raises the possibility of its utility in co-endemic settings where polyparasitism complicates treatment choices. Additionally, the immune-enhancing properties of levamisole warrant further exploration in other parasitic diseases where immune modulation could augment parasite clearance or mitigate pathology.
Despite the promising results, several questions persist. Long-term efficacy beyond the initial follow-up window remains to be established, particularly regarding reinfection rates and the durability of microfilarial suppression. Furthermore, the pharmacodynamics and optimal dosing schedules of levamisole in loiasis require refinement, potentially incorporating biomarkers of immune response to tailor individualized therapy. Safety monitoring will also need to continue, especially in patients with comorbid conditions or concomitant infections common in endemic regions.
The authors acknowledge these caveats and advocate for subsequent Phase IV studies and post-marketing surveillance in real-world settings to validate these findings. Integration with vector control measures and enhanced diagnostic tools, such as rapid microfilarial detection assays, could synergize with levamisole-based therapies to subdue loiasis comprehensively.
In sum, this trailblazing clinical trial elevates levamisole from an obscure candidate to a frontline contender in loiasis treatment. Its short-duration regimens embody a practical, scalable approach aligning with global health imperatives aimed at eliminating neglected tropical diseases. As policymakers and healthcare providers digest these insights, optimism grows for a future where loiasis is no longer a neglected affliction but a curable condition, alleviating human suffering and restoring productivity in some of the world’s most vulnerable populations.
This research exemplifies how revisiting old drugs with modern clinical trial methodologies can rejuvenate the therapeutic arsenal against entrenched diseases. The fusion of strategic pharmacology, rigorous trial design, and a focus on patient safety illuminates a path forward, not just for loiasis, but perhaps as a template for addressing other tropical infections historically sidelined in research agendas.
Looking ahead, continued interdisciplinary collaboration involving parasitologists, immunologists, pharmacologists, and public health specialists will be essential to translate these findings into actionable health policies. Increased funding commitment towards neglected tropical diseases, coupled with in-community advocacy and education, could accelerate the deployment of levamisole regimens, anchoring them in comprehensive disease control frameworks.
In this era of rapid biomedical innovation, the levamisole study reminds us that resolving age-old diseases often requires a blend of scientific perseverance and creative re-examination of existing tools. By doing so, it holds promise to transform healthcare delivery in regions burdened by loiasis, offering not just hope but tangible advances in disease management and eradication.
Subject of Research: Safety and efficacy analysis of levamisole treatment regimens for loiasis
Article Title: Safety and efficacy of 3- and 5-day regimens of levamisole in loiasis: a randomized, placebo-controlled, double-blind clinical trial.
Article References:
Chesnais, C.B., Hemilembolo, M.C., Sahm, B.A. et al. Safety and efficacy of 3- and 5-day regimens of levamisole in loiasis: a randomized, placebo-controlled, double-blind clinical trial. Nat Commun 16, 6191 (2025). https://doi.org/10.1038/s41467-025-61479-6
Image Credits: AI Generated
Tags: 3-day vs 5-day levamisole regimenadverse reactions in loiasis treatmentfilarial nematode infectionshealth burden of loiasisimmunomodulatory agents in medicinelevamisole treatment for loiasisloiasis clinical trial findingsloiasis complications and managementneglected tropical diseases treatmentrandomized placebo-controlled studysafety and efficacy of levamisoletherapeutic outcomes for parasitic infections