In recent years, the diagnosis of thyroid micro-nodules has seen a dramatic increase worldwide, largely driven by technological advancements and heightened public awareness of thyroid health. As these tiny nodules—often measuring less than 10 millimeters—can either be benign or malignant, precisely distinguishing between the two remains a critical challenge for clinicians. Now, a groundbreaking study published in BMC Cancer has demonstrated how machine learning (ML) algorithms combined with dual-layer spectral computed tomography (DLCT) quantitative parameters can significantly improve the accuracy of such distinctions, potentially transforming thyroid cancer diagnosis.
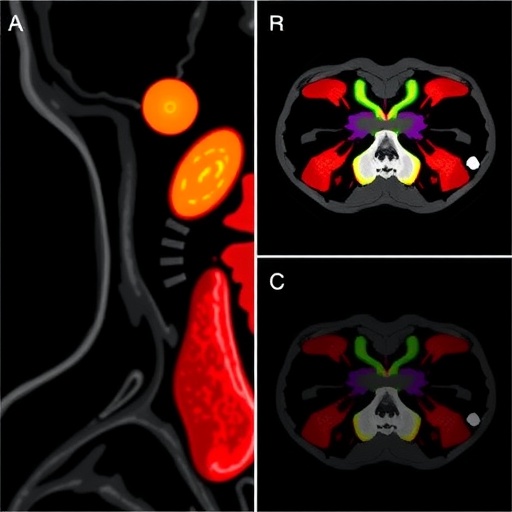
Thyroid micro-nodules represent one of the most frequently detected abnormalities during thyroid screening, but their small size often limits conventional imaging techniques’ ability to differentiate malignant lesions from benign ones. The study led by Song et al. leverages the unique capabilities of DLCT—a cutting-edge imaging modality that harnesses spectral differentiation to extract detailed quantitative data from thyroid nodules. This data, when processed through advanced ML models, allows for unprecedented characterization of nodule pathology.
DLCT captures rich spectral information by simultaneously acquiring high- and low-energy images, enabling fine-grained analysis of tissue composition and vascularization patterns. In this study, 19 quantitative parameters during arterial and venous phases along with four radiological features were measured to represent each thyroid micro-nodule. These parameters provide insights into tissue heterogeneity, iodine uptake, and blood supply, all crucial markers differentiating malignant from benign nodules.
.adsslot_8IewJnCRAE{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_8IewJnCRAE{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_8IewJnCRAE{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The research incorporated a robust dataset comprising 338 thyroid micro-nodules, with 177 confirmed malignant and 161 benign cases. The dataset was meticulously divided into a training cohort of 237 nodules and a testing cohort of 101 nodules. This bifurcation ensured that the ML models developed were both well-trained and rigorously validated on unseen data, permitting an honest estimation of real-world performance.
One of the study’s pivotal methodological strengths lies in its use of recursive feature elimination to select the most informative variables for model training. Instead of relying on the entire set of features, which can introduce noise and reduce accuracy, this technique iteratively removes less significant variables to isolate those most predictive of malignancy. This feature selection optimized the models’ interpretability and clinical applicability.
Three prominent ML algorithms were employed to build predictive models: support vector machine (SVM), logistic regression (LR), and naive Bayes (NB). Each algorithm brings unique strengths to the classification problem. SVMs excel in finding optimal boundaries between classes in high-dimensional spaces, logistic regression offers probabilistic insights with interpretability, and naive Bayes benefits from its probabilistic foundation and efficiency with smaller datasets.
Among these, the SVM model identified six key variables using the “one standard error” rule and demonstrated outstanding diagnostic performance, achieving an area under the receiver operating characteristic (ROC) curve (AUC) of 0.924 in the training cohort and 0.931 in the testing cohort. These values indicate extremely high sensitivity and specificity in distinguishing malignant from benign nodules.
Similarly, the naive Bayes model distilled two principal variables and achieved impressive AUC scores of 0.882 and 0.899 in training and testing cohorts, respectively. Meanwhile, the logistic regression model, with eight key variables, yielded training and testing AUCs of 0.924 and 0.925. Collectively, these results underscore the robustness and reliability of ML models trained on DLCT parameters for thyroid nodule classification.
Beyond individual models, the study developed a total of nine machine learning models with varying combinations of feature sets—2, 6, or 8 variables. Remarkably, all models consistently achieved AUC values exceeding 0.85 across training, cross-validation, and testing datasets, reinforcing the generalizability and clinical promise of this approach.
The clinical implications of these findings are profound. By integrating spectral CT quantitative data with ML algorithms, clinicians could potentially reduce unnecessary biopsies, improve early cancer detection, and tailor patient treatment more precisely. Such advancements align with the ongoing shift towards personalized medicine, where diagnostic tools leverage data-driven insights to enhance outcomes.
Moreover, the use of DLCT represents a non-invasive and rapidly deployable imaging technique readily integrable into existing clinical workflows. Its quantitative parameters, when harnessed through artificial intelligence methods, hold promise for application not only in thyroid micro-nodules but potentially other complex small lesions across various organs.
Importantly, this study exemplifies the transformative potential of combining advanced imaging with artificial intelligence in oncology diagnostics. As AI continues to evolve, its role in interpreting complex datasets, such as spectral CT, will likely expand, driving improvements across cancer detection, staging, and monitoring.
While the results are promising, broader validation on larger multicenter cohorts will be essential to confirm applicability in diverse populations. Furthermore, integration into real-time clinical decision support systems will require optimization for computational efficiency and user-friendly interfaces.
Looking ahead, further refinement of ML algorithms, possibly through deep learning architectures, could capture even subtler patterns in spectral data. Additionally, combining DLCT metrics with other biomarkers or genomic data might enhance predictive power, ultimately enabling more comprehensive thyroid cancer profiling.
In conclusion, the innovative use of machine learning applied to spectral CT quantitative parameters demonstrates a significant leap forward in thyroid micro-nodule diagnosis. By achieving high accuracy in distinguishing benign from malignant lesions, this approach offers a promising path towards earlier detection, better patient stratification, and improved clinical outcomes in thyroid oncology.
Subject of Research: Application of machine learning algorithms to dual-layer spectral computed tomography (DLCT) quantitative parameters for distinguishing benign from malignant thyroid micro-nodules.
Article Title: The value of machine learning based on spectral CT quantitative parameters in the distinguishing benign from malignant thyroid micro-nodules.
Article References:
Song, Z., Liu, Q., Huang, J. et al. The value of machine learning based on spectral CT quantitative parameters in the distinguishing benign from malignant thyroid micro-nodules. BMC Cancer 25, 1041 (2025). https://doi.org/10.1186/s12885-025-14450-z
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14450-z
Tags: advancements in thyroid health technologyartificial intelligence in healthcarechallenges in thyroid micro-nodule diagnosisdistinguishing benign and malignant nodulesdual-layer spectral computed tomographyenhanced imaging techniques for cancer diagnosisimproving accuracy in cancer detectioninnovations in thyroid screening methodsmachine learning in medical imagingquantitative parameters in DLCT imagingspectral differentiation in thyroid nodulesthyroid nodule diagnosis using ML