Hepatitis B virus (HBV) infection has long been recognized as a critical factor associated with the onset of hepatocellular carcinoma (HCC), a primary form of liver cancer that significantly contributes to global cancer morbidity and mortality. Despite this association, the precise mechanisms linking HBV infection to liver carcinogenesis have remained elusive. In a groundbreaking study published in Nature Communications, researchers at Mass General Brigham have elucidated a complex interplay between chronic HBV infection and environmental carcinogens that exacerbates liver inflammation and potentiates cancer development. Their findings challenge traditional views by demonstrating that HBV alone does not directly induce liver cancer or inflammation but rather sensitizes the liver to external carcinogenic insults.
The core revelation of this research lies in the understanding that HBV creates an immunological environment in the liver that amplifies the pathological responses to carcinogens commonly encountered in everyday life, such as compounds present in tobacco smoke, processed meats, fried foods, and alcohol. This synergy between viral infection and environmental factors generates a dysregulated immune response that facilitates neoplastic transformation. Specifically, the study identifies interleukin-33 (IL-33), an inflammatory cytokine, as a crucial mediator in this process, marking a significant advance in comprehending the immune modulation underlying HBV-associated hepatic carcinogenesis.
Utilizing a sophisticated mouse model engineered to mimic chronic HBV infection, the investigators subjected these animals to diethylnitrosamine (DEN), a potent carcinogen reflective of human exposure to common dietary and lifestyle agents. Notably, mice harboring the HBV genome developed severe liver cancer phenotypes only following DEN exposure, whereas HBV presence without the carcinogen failed to provoke significant hepatic injury or tumor formation. This finding underscores the necessity of additional environmental carcinogens in conjunction with HBV to drive hepatocellular cancer initiation and progression.
.adsslot_FE9dWY7H3Q{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_FE9dWY7H3Q{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_FE9dWY7H3Q{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
At the molecular level, DEN exposure in the HBV-infected livers triggered pronounced upregulation of IL-33, a cytokine implicated in chronic inflammation, fibrosis, and tumorigenesis. IL-33’s role as an alarmin positions it as a amplifier of local immune dysregulation, fostering an environment ripe for malignant transformation. This insight prompted the researchers to explore therapeutic interventions aimed at modulating IL-33 activity to attenuate carcinogen-driven liver pathology in the context of HBV infection.
In a promising translational approach, the research team employed pitavastatin, a statin class medication conventionally used for lowering cholesterol, known to exert anti-inflammatory effects including suppression of IL-33 expression. Treatment with pitavastatin in HBV-infected, carcinogen-exposed mouse models effectively diminished IL-33 levels, alleviated hepatic inflammation, and reduced tumor burden. These results suggest a potential adjunctive strategy whereby statins could be integrated with current antiviral regimens to mitigate liver cancer risk among HBV-positive individuals.
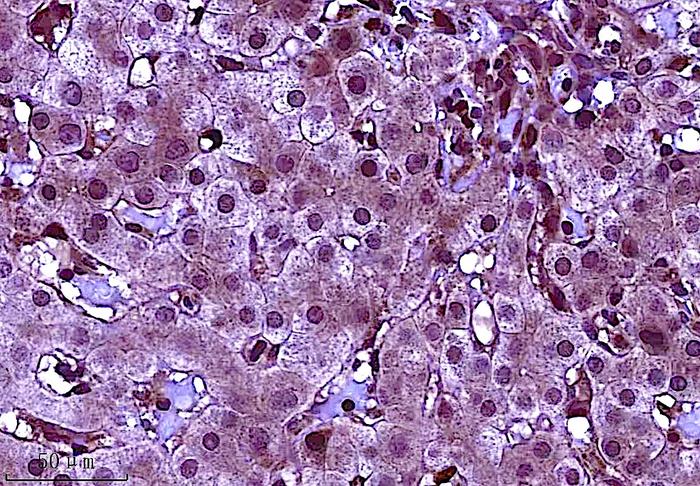
Extending their investigation to human subjects, the researchers performed immunohistochemical analyses on liver biopsy samples from patients with HBV-associated chronic hepatitis compared to healthy controls. Consistent with their animal model data, IL-33 expression was significantly elevated in affected human livers, corroborating the cytokine’s pivotal role in disease pathogenesis. Furthermore, an extensive retrospective analysis involving healthcare data of over 200 million patients revealed that HBV carriers receiving statin therapy exhibited markedly lower incidences of hepatitis flare-ups and liver cancer compared to those administered alternative cholesterol-lowering agents, emphasizing the clinical relevance of their findings.
The implications of this study illuminate the multifactorial nature of HBV-related liver carcinogenesis, highlighting the necessity for integrative therapeutic approaches that not only target viral replication but also modulate inflammatory pathways and minimize environmental carcinogen exposure. This paradigm shift advocates for comprehensive disease management strategies aimed at reducing liver cancer incidence through combined pharmacological and lifestyle interventions.
Dr. Shawn Demehri, lead investigator and principal author from the Demehri Lab and Krantz Family Center for Cancer Research at Massachusetts General Hospital, elaborated on these findings: “Our research redefines our understanding of HBV’s role in liver cancer. The virus acts as a catalyst that alters the hepatic immune landscape, sensitizing the liver to carcinogenic insults and promoting malignant transformation. Targeting inflammation, particularly IL-33, in combination with antiviral therapy, opens new avenues to improve clinical outcomes for patients worldwide.”
This study also cautions against dismissing the influence of diet, tobacco use, and alcohol consumption in HBV-infected populations. Environmental carcinogens, previously considered isolated risk factors, are now demonstrated to synergize profoundly with viral infections to accelerate cancer risk. Public health policies may thus benefit from integrating strict guidelines aimed at reducing carcinogen exposure within at-risk HBV populations.
In addition to pitavastatin, the therapeutic pipeline may explore novel IL-33 inhibitors or agents targeting downstream signaling pathways involved in IL-33 mediated immune dysregulation. Given that statins are widely used and generally well-tolerated, their repurposing for liver cancer chemoprevention holds substantial promise. Prospective clinical trials will be requisite to validate efficacy, determine optimal dosing strategies, and monitor safety profiles specifically within HBV-infected cohorts.
Intriguingly, the study’s findings also carry implications beyond hepatology. Since IL-33 is implicated in diverse inflammatory and fibrotic pathologies, understanding its role in viral-induced carcinogenesis may inspire new research into other virus-associated cancers and chronic inflammatory diseases. The authors disclose a filed patent regarding IL-33 inhibition for treatment of cancer, fibrosis, and inflammation, underscoring the translational potential of targeting this pathway.
In conclusion, the Mass General Brigham research advances the field of liver cancer biology by clarifying the contributory roles of HBV and environmental carcinogens, mediated by immune modulation via IL-33. This integrated model of carcinogenesis paves the way for innovative combination therapies and preventative strategies that may markedly reduce liver cancer burden globally, especially in HBV-endemic regions.
Subject of Research: People
Article Title: Hepatitis B virus promotes liver cancer by modulating the immune response to environmental carcinogens
News Publication Date: 27-Jun-2025
Web References: https://www.nature.com/articles/s41467-025-60894-z
References: Huang M et al. “Hepatitis B virus promotes liver cancer by modulating the immune response to environmental carcinogens” Nature Communications DOI: 10.1038/s41467-025-60894-z
Image Credits: Shawn Demehri, Mass General Brigham
Keywords: Liver cancer
Tags: advancements in cancer research on HBVcancer risk reduction in hepatitis B patientschronic HBV infection and inflammationdietary factors and liver cancerenvironmental carcinogens and liver diseasehepatitis B virus and liver cancerhepatocellular carcinoma risk factorsimmunological environment in liver cancerinterleukin-33 role in liver cancerliver cancer prevention strategiesprocessed meats and liver carcinogenesistobacco smoke and liver health