Adrenomedullin disrupts insulin signaling in blood vessels, leading to systemic insulin resistance in obesity-associated type 2 diabetes, according to a new study by a team at the Max Planck Institute for Heart and Lung Research in Germany. The findings suggest that blocking adrenomedullin’s effects can restore insulin function and improve glucose regulation in a mouse model, suggesting a potential therapeutic target for obesity-related metabolic disease.
This work is published in a paper in Science entitled, “Endothelial insulin resistance induced by adrenomedullin mediates obesity-associated diabetes.” The initial motivation for this study, said Stefan Offermanns, PhD, director and scientific member at the Max Planck Institute for Heart and Lung Research, was to understand the “function of endothelial insulin receptors on a cellular and systemic level both in health and disease.”
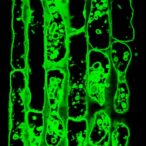
“When insulin binds to its receptor on the endothelium and activates it, this leads to an expansion of the blood vessel diameter and improved permeability of the vessel wall for insulin,” explained first author Haaglim Cho, PhD, project leader at the Max Plank Institute. “As a result, glucose and insulin can be better transported from the blood to metabolically active organs such as the fat tissue and muscles.”
The German team “serendipitously” identified a link between the activation of G-protein coupled receptors and cAMP formation, where the latter inhibits insulin signaling. “Obese mice that lack this signaling pathway in endothelial cells show improved insulin sensitivity and glucose tolerance,” they told GEN. Offermanns also shared that they were initially surprised by this finding, having expected the opposite outcome from their experiment.
Through a series of siRNS-mediated knockdown experiments of likely downstream targets, the team identified adrenomedullin as a promising target for further study. They found increased levels of both adrenomedullin and complement factor H (CFH)—a protein that amplifies the hormone’s effects—in plasma of obese mice and humans.
In experiments using human endothelial cells, the researchers demonstrated that adrenomedullin inhibits insulin signaling by activating a cascade that deactivates the insulin receptor.
Further investigation in vivo, using a mouse model, demonstrated systemic function of adrenomedullin for glucose transport. In contrast to obese mice, lean mice have lower plasma levels of adrenomedullin. Treating the lean mice with adrenomedullin induced insulin resistance and impaired glucose control, mimicking obesity’s metabolic effects.
Genetically engineered mice with impaired production of adrenomedullin or inactivation of its endothelial receptor showed a normal insulin response with adrenomedullin treatment, confirming that the hormone’s action is mediated through these receptors. Blocking adrenomedullin in obese mice showed improved insulin function in blood vessels and prevented insulin resistance.
The authors emphasized that this study “provides additional evidence that endothelial insulin signaling is very important for the systemic action of insulin,” and pointed out that “endothelial insulin resistance in obesity is leading to systemic insulin resistance, which is a new concept.”
Identification of adrenomedullin as a driver of obesity-induced insulin resistance opens the door for research into new therapeutic strategies for treating obesity-associated type 2 diabetes. “Currently the main focus in the scientific community regarding insulin resistance is on the metabolic target organs of insulin such as liver, skeletal muscle, and adipose tissue,” the authors noted.
Treatment options, including GLP-1 receptor agonists, are targeted for insulin production in a precise way. The team is exploring type 2 diabetes from a different angle. “Bringing the endothelial insulin receptor system into the focus of scientific efforts to understand the mechanism of obesity-associated type 2 diabetes will allow us to develop novel therapeutic strategies to reduce insulin resistance in type 2 diabetes based on the novel mechanism described in the study.”
The team will continue their work and shared that they are “currently studying different obese and non-obese human populations with regard to plasma adrenomedullin and CFH levels and the likelihood of these populations to develop type 2 diabetes.”
They further intend to delve deeper into the function of adrenomedullin and its interaction with CFH. “We try to understand better how CFH and adrenomedullin lead to super-activation of the adrenomedullin receptor on endothelial cells as that appears to be a key mechanism,” Offermanns explained.
“We hope that the improved understanding of type 2 diabetes caused by obesity is a first step towards the development of new approaches that can be used to treat type 2 diabetes,” Offermanns concluded.