The results of a preclinical study have identified a biological mechanism that explains why some patients don’t respond to immune checkpoint blockade (ICB) therapy for solid cancer tumors.
The study, by an international group of scientists headed by a team at Newcastle University, also points to a combination treatment strategy for treating ICB-resistant metastatic skin cancers, suggesting that the same approach may also be beneficial in the immunotherapy of other types of solid tumor.
Shoba Amarnath, PhD, Reader in Immune Regulation at Newcastle University, said, “Identifying this mechanism is important as it identifies patients who will not respond to single agent ICB treatment such as anti-PD-1 antibody therapy, but are most likely to benefit from the new combination therapy that we have identified, anti-CD30. By simply adding anti-CD30 for these patients, we can improve their response to cancer and avoid costly delays. Although our work was limited to skin cancer, we believe this new combination treatment will also benefit patients with lung, bowel, pancreatic and other solid cancers who are currently not responding to treatment with ICB monotherapy.”
Amarnath is senior and corresponding author of the researchers’ published paper in Nature Immunology, titled “PD-1 receptor deficiency enhances CD30+ Treg cell function in melanoma.”
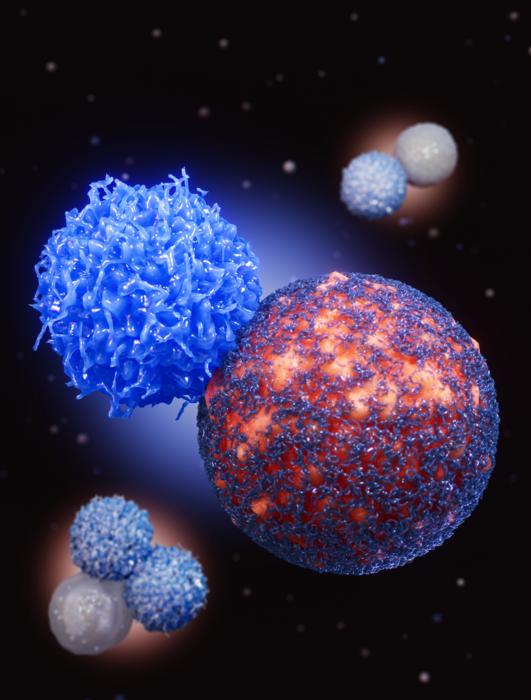
ICB therapy is a type of immunotherapy that aims to unlock the body’s natural immune system to attack cancer cells. It works by targeting and blocking specific “checkpoints” in the immune system, such as PD-1, that normally help to keep it in check, allowing T cells to recognize and destroy cancer cells more effectively.

The use of immune checkpoint blockade (ICB) therapy in solid cancers has shown unexpected success in a significant minority of patients. However, resistance to ICB therapy affects more than 60% of cancer patients who are prescribed this kind of treatment, which can cause significant toxicity in non-responders.
Through their newly reported study, Amarnath and colleagues demonstrated that ICB resistance occurs due to the treatment’s effect on regulatory T cells (Tregs). Regulatory T cells are a subtype of CD4+ T helper cells that restrain the immune system, and this immune cell type expresses a number of inhibitory coreceptors, such as PD-1.
The use of antibodies to PD-1 and its ligand PD-L1 has been successful in the treatment of several cancers, the team continued, “… yet many cancer patients do not respond to this treatment, and in some cases PD-1 inhibition may enhance cancer growth … Emerging literature suggests that anti-PD-1 immunotherapy can counterintuitively enhance Treg cell numbers in a proportion of patients, driving resistance to immunotherapy.” The underlying mechanisms that fuel this resistance within the immune system aren’t yet clear.
To investigate ICB resistance, the researchers turned to a new engineered mouse model in which PD-1 deficiency is limited to Treg cells and also investigated samples from human skin cancer patients. The new mouse model was engineered by scientists at Newcastle University to specifically allow understanding of ICB resistance.
Through their experiments the team found that ICB therapy enhances the expression of several alternate checkpoint proteins in Tregs that contribute to enhanced cancer growth. And importantly, they discovered that CD30 plays what they describe as a central role within this network in facilitating Treg cell suppressive function within the tumor microenvironment (TME). The studies confirmed that CD30 expression in human Treg cells is driven by blockade of the PD-1/PD-L1 pathway.
“These data indicate a role for PD-1 as a checkpoint that negatively controls CD30 expression in Treg cells to limit their suppressive function,” they noted. “In the absence of PD-1, an increase in specific coinhibitory receptor expression is noted that enhances Treg cell function within the tumor microenvironment … Treg cells cultured in the presence of an anti-PD-L1 antibody showed upregulation of CD30 for all three human melanoma patients suggesting that it is not the TME but anti-PD-1 activity that drives CD30 expression in tumor Treg cells.”
And when investigating whether CD30 might be used as a biomarker for predicting cancer-free survival, the results indicated that high CD30 expression in peripheral blood mononuclear cells “… was associated with poor survival in patients with uveal melanoma and those with breast, lung or colon cancer, indicating that CD30 could be used as a biomarker and therapeutic target that may determine disease outcomes after checkpoint therapy.”
Amarnath added, “Further progress in the laboratory has discovered new immune specific proteins and tumor growth proteins that have elevated expression in Tregs during ICB therapy. We also found that these Tregs show stem-cell like properties.” Ongoing work in the laboratory includes understanding the function and potential therapeutic value of targeting these new proteins in Tregs in skin and other solid cancers.
“We are very excited to find all these new aspects in ICB resistance biology which will not be possible without this new murine model. We believe targeting immune molecules and tumor growth proteins will significantly enhance the efficacy of ICB in solid cancers,” Amarnath continued.
In the paper the researchers described how targeting CD30 can rescue, or overcome, checkpoint therapy resistance in skin cancer. Interestingly, they separately pointed out that an anti-CD30 antibody drug conjugate (ADC) brentuximab vedotin (BV) is already available for treatment of blood cancers, and the investigators suggest this has potential to be used in combination therapy for other tumor types.
Amarnath pointed to results from a Phase II study evaluating combination therapy using BV and anti-PD-1 ICB against metastatic non-small cell lung cancer (NSCLC) and metastatic cutaneous melanoma patients who don’t respond to PD-1 ICB monotherapy. The trial data showed that combination treatment resulted in what the authors of that study, reporting in their paper, called “encouraging” overall survival and progression free survival. “BV + pembrolizumab in solid tumor malignancies resulted in clinically meaningful, durable responses with encouraging OS and PFS rates supportive of the immunomodulatory activity of this combination,” they noted in that paper.