A new material developed at Cornell University could significantly improve the delivery and effectiveness of mRNA vaccines by replacing a commonly used ingredient in lipid nanoparticles (LNPs) that may trigger unwanted immune responses in some people. Traditional lipid nanoparticle formulations for mRNA delivery contain the polymer poly(ethylene) glycol (PEG), which is widely used in drug delivery carriers, but has recently been linked to immunogenicity concerns.
Cornell University professor of biomedical engineering Shaoyi Jiang, PhD, and colleagues have now developed poly(carboxybetaine) PCB lipids as surrogates for PEG-lipids used in mRNA formulations. Preclinical in vitro tests and in vivo immunization studies in mice showed that the PCB-containing LNPs had greater therapeutic efficacy than their PEG counterparts and could be administered repeatedly without loss of efficacy.
Senior and corresponding author Jiang and colleagues reported on their developments and studies in Nature Materials, in a paper titled “Poly(carboxybetaine) lipids enhance mRNA therapeutics efficacy and reduce their immunogenicity,” in which they concluded, “Overall, these findings highlight PCB-containing LNPs as a potent and safe mRNA delivery platform for clinical applications.”
Thanks to their ability to train cells to produce virus-killing proteins, mRNA vaccines have gained popularity over the last five years for their success in reducing the severity of COVID-19 infection. The delivery vehicle for an mRNA vaccine needs to strike a Goldilocks balance—stable enough to protect the mRNA, yet labile enough to release it inside cells, and shielded enough to evade immune surveillance, but not so hidden that it hinders cellular uptake.
One method for delivering the mRNA to cells is by packaging it inside fatty spheres, the lipid nanoparticles that protect the mRNA from being degraded. “Successful implementation of messenger RNA (mRNA) COVID-19 vaccines is greatly credited to the development of lipid nanoparticles (LNPs) that protect mRNA from degradation and ensure effective cellular uptake and mRNA endosomal escape,” the authors wrote. In the LNP system, PEG provides what the team describes as “a stealth coating to the particles to avoid aggregation during the self-assembly process and storage.” PEG increases the stability of LNP particles in the body and so help to avoid rapid clearance, they added.
The PEG component of such lipid nanoparticles may present some unintended side effects in a small subset of individuals, provoking immune responses. “… recent studies have correlated the unwanted allergic effects of LNP vaccines with PEG-related immunogenicity,” the team stated. Researchers have in addition reported accelerated blood clearance (ABC) in LNPs after repeated dosing in mouse studies, leading to loss of efficacy due to the induction of anti-PEG antibodies. Scientists have accordingly been searching for more biocompatible materials. “… exploring alternatives to PEG-lipids is underway to mitigate potential immunogenicity concerns,” the investigators wrote.
Jiang and colleagues have been working to replace the PEG component of lipid nanoparticles with a more adaptable and stealthy option. “The human body is mostly water, so if you insert something with exposed hydrophobic moieties, like PEG, into our blood stream, our immune surveillance system says, ‘Hey, that’s a foreign material,’ and will generate an antibody to destroy it,” Jiang said. This environment makes adverse responses to a vaccine more likely and thus makes it harder for the vaccine to do its job.
Most people’s immune systems are already primed to fight PEG. Prior research shows that a majority of people have anti-PEG antibodies “from people being exposed to PEG in so many commercial products like shampoo and toothpaste,” said Jiang, adding that this widespread exposure may explain why the body is so quick to flag PEG as a threat.
To solve this, Jiang developed lipid nanoparticles that use a zwitterionic polymer, a crucial alternative to PEG, enhancing performance and biocompatibility. Due to the super-hydrophilic—water-loving—nature of zwitterions, this material is able to blend into the body and deliver the mRNA more easily. This specific naturally derived material, poly(carboxybetaine), PCB, has perfect balance of stealth and stability. PCB has previously been used in various carriers, including polyplexes for delivering DNA, and lipoplexes for small interfering RNA (siRNA) delivery, the authors pointed out.
“PCB has been applied in various biomedical applications, such as protein conjugates and nanoparticles, to replace PEG and address the immunogenicity of PEG that can hinder drug efficacy,” they continued. In their newly reported paper, the researchers found that replacing the PEG component of lipid nanoparticle using PCB results in highly effective mRNA vaccines that do not adversely trigger the body’s immune system.
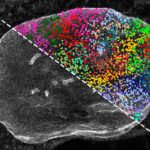
The zwitterionic nanoparticles help sneak the vaccines past the body’s immune surveillance so that they induce antigen-specific immune responses while minimizing undesired immune activation. The team’s studies showed that their PCB-containing LNP formulations exhibited a safe immunotoxicity profile and mitigated the accelerated blood clearance effect previously observed for PEG-containing LNPs, enabling repeated administration loss of efficacy. “Significantly, PCB-containing LNPs (PCB-LNPs) achieve higher transfection efficiency with minimal toxicity than LNP formulations with PEG (PEG-LNPs),” the authors stated. “Overall, we introduced PCB-lipids as a replacement for PEG counterparts in LNPs, enabling enhanced mRNA transfection and repeated administration for various clinical applications.”
Jiang is working with Weill Cornell Medicine, Houston Methodist Cancer Center, the Hospital for Sick Children in Toronto, and the National Cancer Institute to move this discovery toward clinical applications, specifically in the development of mRNA-based cancer vaccines. “With a virus like COVID-19, you only need a tiny vaccine dose, and our immune system will respond. But for a cancer vaccine, the tumor environment suppresses the immune system, so you need a much higher dose to be effective,” said Jiang. “If a patient has a minor problem because of the PEG, the issue will be amplified with a higher dose.”