Dengue, a mosquito-borne viral disease that infects an estimated 100 million people globally each year, is notorious for its unpredictable severity. Some people experience little more than a fever and rash, while others progress to life-threatening bleeding or organ failure. Now, a new study led by Duke-NUS Medical School in Singapore reveals that the virus can leave a lasting genetic “imprint” on the immune system—one that reshapes how people respond to future infections and vaccines.

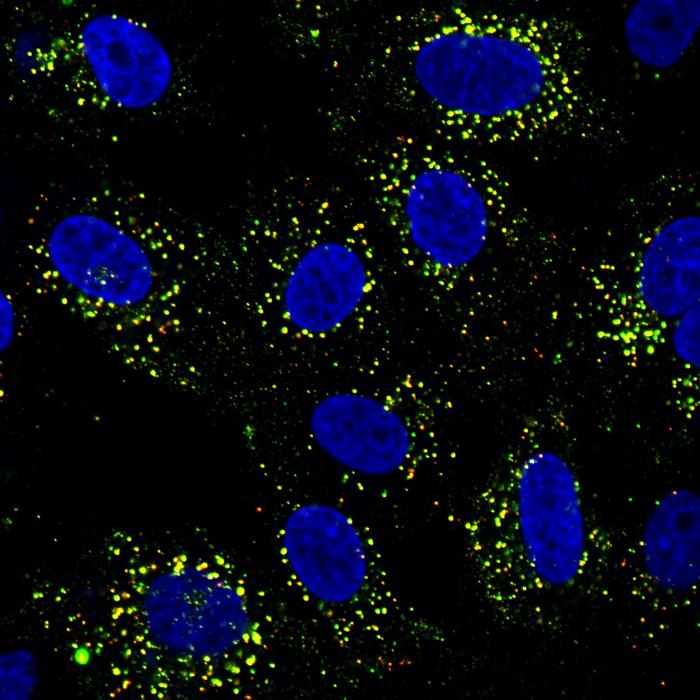
The study, published in Med and titled “Dengue virus infection reprograms baseline innate immune gene expression,” shows that, unlike vaccination, natural dengue infection reprograms innate immune cells. This trained immunity may help explain why vaccines work better in people with prior exposure to the virus.
Infection versus vaccination
Researchers analyzed blood samples from volunteers in the United States. Participants received Takeda’s TAK-003 dengue vaccine in a clinical trial, and their immune responses were compared to those who had previously been infected with dengue. “To understand the underpinnings of the difference in antibody response to TAK-003 [live-attenuated tetravalent dengue vaccine] vaccination in baseline seronegative and seropositive individuals, we profiled whole-blood mRNA using a full-genome microarray. The number of differentially expressed genes (DEGs) and their expression kinetics were both qualitatively and quantitatively different between seronegative and seropositive subjects after the first of two TAK-003 doses,” wrote the authors.
Later on, the researchers expanded the study to Singapore: “To ensure that our findings were not biased by a single small cohort, we included two separate prospectively enrolled cohorts of healthy volunteers in Singapore. The first cohort (enrolled by Kalimuddin) included healthy volunteers in a study on the host response to the live-attenuated yellow fever vaccine (YF17D-204), and the second (enrolled by Low) had healthy volunteers who participated in a study to validate baseline transcriptome differences observed from the DEN-210 cohort. Anti-dengue immunoglobulin (Ig)G ELISA was used to differentiate volunteers into seropositive or seronegative for dengue.
They found that even before vaccination, dengue-experienced individuals displayed distinct gene activity patterns. “Our findings show that natural dengue infection can leave a lasting genetic imprint on the immune system,” said Eugenia Ong, PhD, principal research scientist at Duke-NUS and first author of the study. “Instead of returning to normal, the immune system resets into a new baseline—one that may explain why second infections are often more severe.”
Why vaccines work better post-infection
This immune “reset” means that in people who had prior dengue infection, a single dose of the vaccine triggered stronger antibody responses than two doses did in dengue-naïve individuals. As the authors wrote in Med, “while a single DENV infection reprogrammed the gene expression of innate immune markers…vaccination did not show evidence of similar innate immune reprogramming.”
Senior author Eng Eong Ooi, PhD, from the Emerging Infectious Diseases Program at Duke-NUS Medical School, compared the phenomenon to athletics: “Think of it as training for a sport—the immune system only gets a real workout from the full game—the equivalent of a natural infection. A light warm-up from vaccination isn’t enough to reprogram it.”
Implications for vaccine strategy
The findings clarify why dengue vaccines are more effective in individuals who have already had dengue. They also highlight why an “imperfect” vaccine can still be used safely to reduce disease burden.
Patrick Tan, MD, PhD, professor and senior vice-dean for research at Duke-NUS, emphasized the broader significance: “As dengue continues to affect millions across Asia, Latin America, and other tropical regions, this study closes a critical gap in our understanding of how infection reshapes the immune system. These insights are vital not only for developing better vaccines but also for guiding global and national health policies.”
By identifying how dengue alters innate immunity, the study paves the way for designing next-generation vaccines that can mimic the infection’s imprint without the risks of disease. While researchers caution that a perfect dengue vaccine may still be a decade away, their findings strengthen the case for deploying current vaccines to safely prevent millions of cases worldwide.