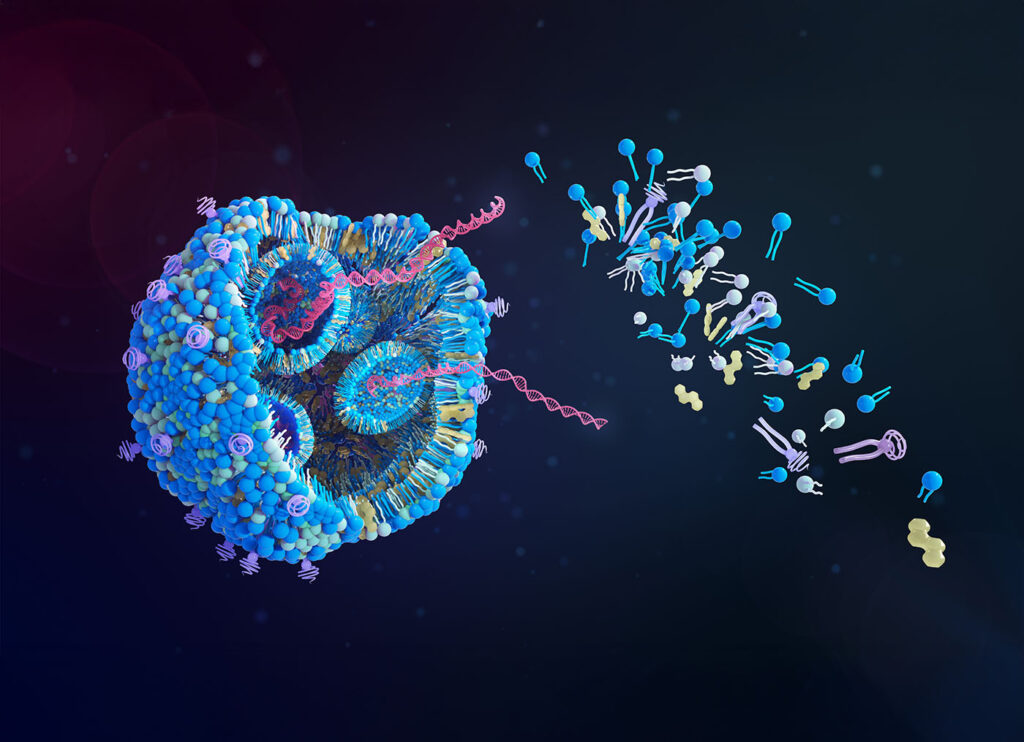
Credit: Tumeggy / Science Photo Library / Getty Images
Lipid nanoparticle (LNP) mRNA vaccines induce robust immune responses and provide protection against infectious diseases. However, this immunity can be short-lived, resulting in the need for frequent booster vaccinations.
In a new study published in Science Immunology titled, “An Il12 mRNA-LNP adjuvant enhances mRNA vaccine–induced CD8 T cell responses,” researchers from the University of Pennsylvania (Penn) found that adding a cytokine produced by various immune cells, known as IL-12, to mRNA vaccines enhanced T-cell response against SARS-CoV-2 and influenza for longer lasting protective effect. The vaccine also improved protection in a mouse melanoma model, offering a potential approach for reducing the risk of cancer.
Anthony Phan, PhD, a postdoctoral researcher at Penn and co-lead author, said one practical aspect of an IL-12 mRNA vaccine is being able to reduce the frequency and amount of vaccine.
“Anything that can be used to reduce injection frequency and dose-related adverse events is a good thing, and so this allows us to think about that as a strategy,” said Phan.
Susan Domchek, MD, director of the Abramson Cancer Center’s Basser Cancer Interception Institute, which provided funding for the study, said cytokine mRNA is “clearly a promising and clever approach to enhance immune stimulation against cancer and pre-cancer lesions.”
“We are hopeful this technology can move as fast as possible into the clinic for patients and individuals at risk of cancer,” she continued.
IL-12 is naturally produced by the body in response to many infections. Researchers have utilized IL-12 as a vaccine adjuvant to promote immunity against parasitic, viral, and bacterial infections.
Designing vaccines that induce strong responses from CD8+ T cells has historically been a challenge, but mRNA vaccines offered a game changer. Data from the last four years show that people who generate strong T-cell responses from the mRNA-based COVID-19 vaccines are less likely to get breakthrough infections or become hospitalized.
Christopher Hunter, PhD, distinguished professor of pathobiology at the School of Veterinary Medicine at Penn and corresponding author of the paper, said the study came together through his lab’s interest in cytokine biology and Phan’s particular interest in CD8+ T cells.
Additional influencers included the work of Drew Weissman, MD, PhD, 2023 Nobel laureate and director of the Penn Institute for RNA Innovation, on vaccine development, and the expertise of Penn Medicine assistant professor Mohamad-Gabriel Alameh, PhD, on particle design, production, and development of vaccines against bacterial pathogens.
“This is why you’re at a university, so you can meet people that you don’t usually interact with, and you find common interests,” said Hunter. Alameh, who met Hunter and Phan on campus, said he quickly realized that combining cytokine-based immune modulation and material engineering is the best route to tailor vaccine responses.
Looking ahead, the research team is exploring the impact of other cytokine mRNAs that can be used to modulate the immune response and whether IL-12 could improve vaccine candidates for HIV. In addition, ongoing research with Scott Hensley, PhD, professor of microbiology at Penn Medicine, is focused on the ability to deploy this approach across species for avian influenza.