Los Angeles, CA – In a groundbreaking advancement for brain cancer research, scientists at the Terasaki Institute for Biomedical Innovation (TIBI) have unveiled an innovative three-dimensional (3D) microphysiological system that models chemoresistance in glioblastoma (GBM) by incorporating the critical role of pericytes. Spearheaded by Dr. Vadim Jucaud, Assistant Professor at TIBI, this novel in vitro platform replicates not only the cellular complexity of the GBM microenvironment but also faithfully reproduces the biomechanical and physicochemical attributes of human brain tissue, offering a significant leap forward in accurately studying drug response and resistance mechanisms in this dreadful malignancy.
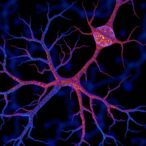
Glioblastoma remains one of the most aggressive and lethal brain tumors, with patient prognosis barely improving over recent decades despite advancements in therapeutic interventions. Standard chemotherapy treatment employing temozolomide (TMZ) frequently encounters resistance, a challenge that has perplexed oncologists and researchers alike. Recognizing the crucial influence of the tumor microenvironment in GBM pathology, Dr. Jucaud and colleagues engineered a biomimetic 3D system that seamlessly integrates human GBM tumor cells with pericytes, specialized supportive cells found around brain vasculature, within a meticulously designed biomaterial scaffold that emulates the brain’s unique mechanical stiffness and transport properties.
This system transcends traditional two-dimensional cultures by creating a multi-cellular environment that closely mirrors in vivo tumor dynamics. The model was applied across three distinct GBM cell lines co-cultured with primary human pericytes, revealing a marked increase in TMZ resistance ranging from 22% to greater than 32% when pericytes were present. Crucially, this chemoresistance was mechanistically tied to a striking 160-fold upregulation in pericyte-derived CCL5, a chemokine implicated in inflammatory signaling, cellular survival pathways, and drug resistance, thus identifying a potent signaling axis that could serve as a therapeutic target.
Dr. Jucaud emphasized the importance of replicating tissue-level mechanical properties, stating that their 3D model “provides a more accurate framework to study drug response and resistance than previously achievable in vitro systems.” By faithfully emulating both cellular interactions and biomechanical cues, this platform enables the dissection of complex tumor-stroma cross-talk that drives chemoresistance—a critical step towards developing therapies that can overcome this barrier and improve clinical outcomes.
Furthermore, the study highlighted the differential sensitivity of various GBM cell lines to TMZ, noting that some lines exhibited significant off-target toxicity, an observation underscoring the heterogeneity of tumor responses within patients. This personalized aspect of the model supports its utility for precision medicine approaches, allowing for high-throughput screening of existing and novel chemotherapeutic agents under conditions that exceptionally replicate the in vivo tumor microenvironment.
The implications of this work extend beyond fundamental cancer biology. As Dr. Ali Khademhosseini, CEO of TIBI, points out, “This model represents a powerful preclinical tool that captures key elements of tumor biology often overlooked in simpler systems. It opens the door to more accurate drug screening and a better understanding of resistance mechanisms in GBM.” By leveraging the platform’s ability to closely mimic the physical and biochemical tumor niche, researchers can expedite the discovery of efficacious therapeutics and tailor treatments to individual patient profiles.
Notably, this biomimetic platform offers a scalable and cost-effective alternative to traditional animal models, which are often time-consuming and limited in their ability to recreate human tumor complexity. The engineered system supports high-throughput experimentation, making it an invaluable resource not only for academia but also for pharmaceutical companies engaged in oncology drug development and screening programs.
From an engineering perspective, the biomaterial scaffold utilized in the system was carefully designed to replicate key physical properties such as matrix stiffness, porosity, and diffusivity, which are known to influence tumor cell behavior and drug penetration. Such mechanical fidelity allows the system to reproduce the dynamic physical constraints of the brain tissue, contributing to an authentic representation of tumor microenvironmental stressors.
Biologically, the pronounced role of pericytes in this chemoresistance model underlines the importance of vascular-supportive cells in tumor progression. By secreting CCL5 and potentially other signaling molecules, pericytes facilitate a protective niche for GBM cells, thereby reducing the efficacy of TMZ. Targeting this axis may therefore represent a viable therapeutic avenue to sensitize tumors and curtail resistance development.
The study, recently published in Acta Biomaterialia, marks a significant milestone in the intersection of tissue engineering, cancer biology, and translational medicine. It showcases how the convergence of advanced biomaterials and cellular co-cultures can propel disease modeling to new heights, bringing us closer to elucidating the multifaceted nature of cancer and overcoming therapeutic roadblocks.
As the field moves toward more physiologically relevant models, platforms like the one developed by Dr. Jucaud and colleagues will undoubtedly reshape the landscape of preclinical research. By honing our understanding of how the tumor microenvironment—especially pericyte interactions—modulates drug resistance, this innovation not only promises to catalyze the development of smarter treatments but also ignites hope for patients afflicted with glioblastoma worldwide.
Subject of Research: Lab-produced tissue samples
Article Title: Microphysiological system modeling pericyte-induced temozolomide resistance in glioblastoma
News Publication Date: 27-May-2025
Web References: Terasaki Institute for Biomedical Innovation
References: DOI: 10.1101/2024.07.16.603611
Image Credits: Terasaki Institute
Keywords: Glioblastoma cells, Brain cancer, Pericytes, Tumor microenvironments
Tags: 3D microphysiological modelbiomimetic scaffold for glioblastomabrain cancer drug responseglioblastoma research advancementsin vitro brain tissue modelinginnovative cancer treatment strategiesmechanobiology of brain tumorsmulti-cellular tumor modelspericyte-driven chemoresistancetemozolomide resistance mechanismsTerasaki Institute for Biomedical Innovationtumor microenvironment in GBM