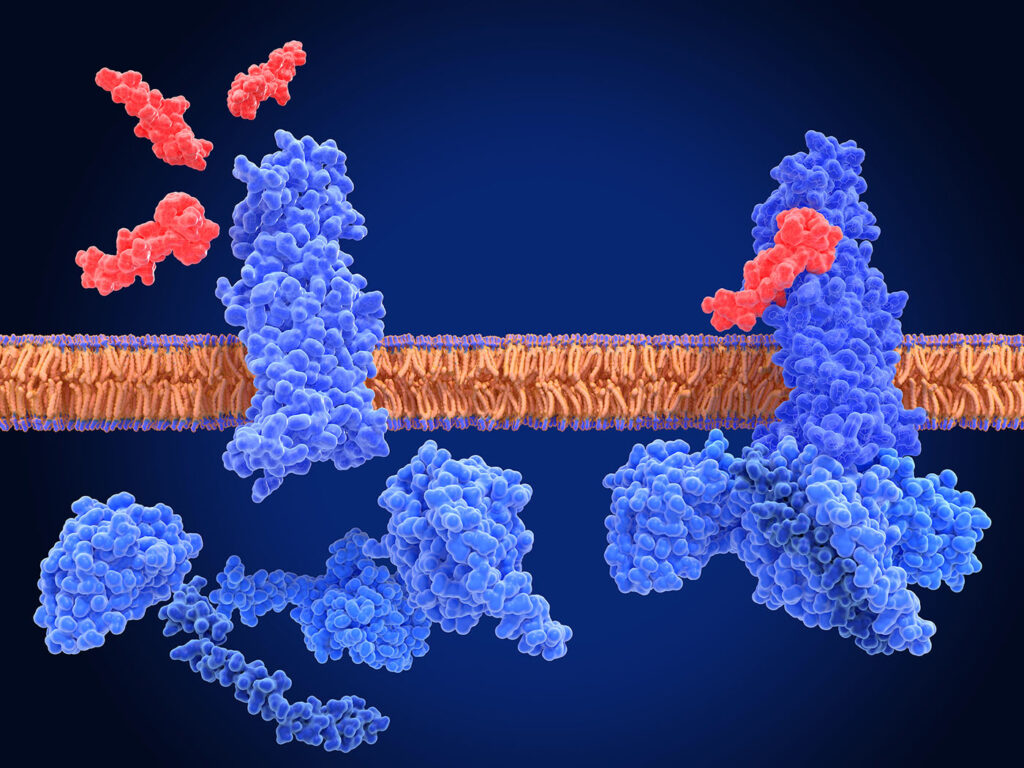
If cells are the factories, proteins are the workers. They control nearly every aspect of cell function, from structure to signaling, from transport to defense. And, like many workers, they rarely act alone. Physiochemical protein-protein interactions (PPI) drive biological functions.
However, when things go awry, such as a genetic mutation or a misfolding, diseases can arise. And because these changes are often in a key component that drives and regulates cell function, the resulting disease can be difficult to treat. One common approach is to inhibit these proteins from connecting with their binding partner. For example, there are currently 85 FDA-approved kinase inhibitors targeting around two dozen different proteins, such as epidermal growth factor receptor (EGFR) and cyclin-dependent kinase (CDK) 4/6.1
But there are many other proteins and specific genetic mutations with no treatment options, including some responsible for fatal neurological disorders and advanced cancers that have long been considered “undruggable.” These indications have required further innovation, such as the novel platforms and therapeutics being developed by the companies described here.
Expanding the arsenal of RAS and KRAS inhibitors
Cell proliferation is largely dictated by a group of small proteins called the RAS family, which act as molecular switches between “ON” and “OFF” states. However, genetic mutations in the RAS gene often result in excessive RAS(ON) growth signaling, driving cancer development.
“Oncogenic RAS mutations are among the most common drivers of human cancers, and are often associated with poor survival outcomes,” says Mark Goldsmith, MD, PhD, CEO and chairman of Revolution Medicines. “Mutant RAS has long been considered a recalcitrant drug target due to its featureless surface and bias toward the RAS(ON) state that, historically, has been even more difficult to drug with small molecules.”

To address that challenge, Revolution Medicines has developed a tri-complex inhibitor platform in which molecules bind to a chaperone protein and “form a novel binary interface with high affinity for RAS(ON),” explains Goldsmith. With this platform, they can target all of the most common forms of oncogenic RAS(ON), including those with mutations at the three most commonly mutated hotspots—G12, G13, and Q61.
There are currently two global Phase III studies underway for their most advanced RAS-targeting investigational drug, daraxonrasib, a multi-selective inhibitor. RASolve 301 is comparing daraxonrasib to chemotherapy in patients with previously treated, locally advanced or metastatic RAS mutant non-small cell lung cancer (NSCLC). And, RASolute 302 is a monotherapy trial of daraxonrasib in patients with previously treated pancreatic ductal adenocarcinoma (PDAC) harboring a RAS mutation.
An analysis of preliminary safety and activity data from two Phase I studies of daraxonrasib was reported in December 2024. “Patients with PDAC harboring a RAS G12X mutation achieved a median progression-free survival (PFS) of 8.8 months… and patients with PDAC harboring any RAS mutation achieved a median PFS of 8.5 months,” says Goldsmith. Similarly, patients with previously treated RAS mutant NSCLC demonstrated encouraging antitumor activity, with a median PFS of 9.8 months, a median overall survival (OS) of 17.7 months, and an objective response rate (ORR) of 38%.
Revolution Medicines is also developing RAS(ON) inhibitors that target specific G12 mutations. Zoldonrasib, a G12D-selective covalent inhibitor, has demonstrated acceptable tolerability and encouraging antitumor activity in initial data from a Phase I study in patients with NSCLC. And, elironrasib, a G12C-selective covalent inhibitor, is being explored as a combination therapy in clinical studies with patients with NSCLC.
Both zoldonrasib and elironrasib were designed for patients with a KRAS mutation. These are one of the most common gene mutations linked to cancer, present in about 25% of tumors, particularly pancreatic, colorectal, and lung cancers.2 However, it has taken nearly four decades since its discovery as an oncogene for researchers to locate targeting sites on the KRAS protein.

“KRAS is a relatively small protein with no obvious binding pockets in the apo state (not bound to its co-factors). In addition, its co-factors are binding with high affinity, and therefore pose a high hurdle for small drugs competing with these endogenous binding partners,” says Peter Ettmayer, PhD, head of drug discovery sciences at Boehringer Ingelheim in Vienna. While “innovative approaches like ‘warhead first’ and ‘fragment-based finding’ led to the approval of the first drugs targeting the KRASG12C mutation… 85% of all KRAS-mutated cancers still lack novel agents.”
Boehringer Ingelheim, in collaboration with Alessio Ciulli, PhD’s lab at University of Dundee, discovered a KRAS degrader, ACBI3, that can target a much wider range of KRAS-mutated cancers. Preclinical experiments have found that this small molecule “takes out 13 of the 17 most common forms of mutated KRAS,” says Ettmayer, which covers a wide range of tumor types. At the same time, it’s highly selective. In a panel of 300 cancer cell lines, ACBI3 was broadly active in cell lines containing KRAS mutations, while sparing those without them.
In addition, compared to inhibition, ACBI3 “enables a greater than 10-fold higher potency… and results in prolonged suppression of uncontrolled cell proliferation.” This high efficacy has led to a tumor regression in RKN (KRAS G12V) tumor-bearing mice. Scientists can access the degrader free of charge via Boehringer’s open innovation portal opnMe.
A first-in-class molecular glue degrader
In addition to RAS and KRAS, casein kinase 1 alpha (CK1a) is another protein that plays a critical role in many biological processes and has been linked to cancer development. Yet, “Despite extensive efforts, the development of selective CK1a inhibitors has been largely unsuccessful due to its structural similarities with other kinases in the [casein kinase superfamily],” explains Hyunsun Jo, PhD, CEO of Pin Therapeutics.
“However, Pin Therapeutics has demonstrated that CK1a can be selectively degraded using targeted protein degradation (TPD) technology,” he continues. The company has developed new molecular glue degraders (MGD) that selectively bind to a target protein, facilitating the interaction between the target and an E3 ligase with a CRBN substrate that degrades the target. Through this technology, they have developed an orally available, molecular glue degrader, PIN-5018, that targets CK1a in patients with solid or blood tumors.

In preclinical in vivo studies as a monotherapy, PIN-5018 led to broad tumor growth suppression in microsatellite-stable colorectal cancer (MSS-type CRC) across multiple PDX models, showed efficacy independent of hormone-blocking or androgen receptor signaling in castration-resistant prostate cancer (CRPC) models, and contributed to complete remission in aggressive PDX adenoid cystic carcinoma (ACC) models. In the wake of these promising results in cancers with limited therapeutic options, in May, PIN-5018 received clearance for a Phase I clinical trial in patients with solid tumors.
Noting its differentiated mechanism, translational foundation, and strategic targeting of high-need cancers, Hyunsun says that as PIN-5018 “advances toward the clinic, it represents not only scientific progress but also a renewed sense of possibility for patients and providers alike.”
Making larger molecules to target a larger binding site
Another group of proteins implicated in cancer development are CDKs, which form a complex with cyclin proteins. To date, there are four FDA-approved CDK 4/6 inhibitors—small molecules that bind to the kinase active site of CDKs, causing cancer cells to arrest in the cell cycle.

But there’s a binding site on the cyclin proteins that, until recently, hasn’t gotten as much attention. This site, called the hydrophobic patch, is where some key proteins first bind to, like RB1 and E2F. The scientists at Circle Pharma believe that targeting the hydrophobic patch, rather than the kinase active site, offers the potential for more selectivity, safety, and the opportunity to not just stop tumor cells from proliferating, but to actively kill them. That is, if it can be targeted.
“For over 25 years, the hydrophobic patch of the cyclins has been seen as undruggable,” says David Earp, JD, PhD, president and CEO of Circle Pharma. “When these substrate proteins, like RB1 and E2F, come to bind to the complex, they first interact with this large, flat hydrophobic patch. The energetics of the interaction are spread out over a large surface area, and so a small molecule is just not going to be effective.”
Instead, Circle Pharma created large molecule macrocycles that can target what small molecule drugs cannot. And, despite their larger size, they can be delivered orally as well.
“We’re the only company that’s been able to develop a modality—a macrocycle, in this case—to drug the hydrophobic patch,” says Earp. Their lead candidate, CID-078, an oral cyclin A/B RxL inhibitor, is more than twice the size of typical small molecule drugs and has exhibited promising preclinical results.
For instance, in a study using an ER+ breast cancer PDX mouse model, they found that “all three dosing regimens tested produce a profound shrinkage of the tumor to the point where it’s no longer measurable,” says Earp. “This is what we are hoping that we’re going to be able to see in the clinic, this clear, single agent tumor shrinkage.”
CID-078 has recently advanced to Phase I clinical trials in patients with advanced solid tumors. In addition, Circle’s second program, oral macrocycles that inhibit the oncogene cyclin D1, has demonstrated favorable preclinical in vivo responses, and Circle expects to file an IND in 2026. And, in October 2024, they announced a collaboration with Boehringer Ingelheim in which they will use their MXMO platform to target another cyclin implicated in the growth of cancer cells.
Eliminating disease-causing extracellular proteins at their source
Beyond cancer-causing proteins, misfunctioning extracellular proteins can cause a variety of diseases, including autoimmune and neurodegenerative diseases. Current methods for eliminating disease-causing extracellular proteins have some major limitations. For instance, RNA targeting works well only if the offending protein is in the liver, and neutralizing antibodies have trouble targeting proteins after they’re made and eliminating protein aggregates.
Instead, Gate Bioscience is developing molecular gates that can eliminate disease-causing extracellular proteins before they leave the cell.

“As the protein is being produced coming off the ribosome, as it’s entering the secretory translocon, it’s that first committed step on its journey to getting outside the cell—we block it at that step,” explains Brian Cathers, PhD, CSO of Gate Bioscience. “As far as we can tell, what it’s doing—blocking translocation—causes that protein to spool up into the cytoplasm instead of entering the ER lumen. It’s recognized as being mislocalized, and natural cellular machinery eliminates the mislocalized proteins.”
While these small molecules won’t directly affect already formed proteins and aggregates, by stopping more from forming it gives other medications more time to take effect. The company is focusing on toxic secreted protein-type diseases. In a collaboration with the Broad Institute, they are currently working on an orally available molecular gate for Creutzfeldt-Jakob disease (CJD), a fatal neurodegenerative disorder caused by prions, or misfolded proteins.
“We’ve shown effective target engagement in an in vitro setting, and recently, we demonstrated target engagement in vivo,” explains Cathers. “Just last month, we actually, for the first time, disclosed efficacy in a CJD animal model.” They hope to begin human testing in the next two years.
References
- Roskoski R. Properties of FDA-approved small molecule protein kinase inhibitors: a 2025 update. Pharmacol Res. 2025;216:107723. doi:10.1016/j.phrs.2025.107723.
- Chien S. Targeting the KRAS mutation for more effective cancer treatment. MD Anderson Cancer Center.