In a groundbreaking multicenter study poised to reshape breast cancer treatment strategies, researchers have unveiled new insights into the capabilities of [18F]FLT PET/CT imaging in predicting tumor response to neoadjuvant chemotherapy (NAC). This retrospective analysis leverages a rich dataset from the ACRIN 6688 observational trial, offering a comprehensive examination of how the tumor to background parenchymal ratio (TBR) of standardized uptake values (SUV) can provide critical prognostic information for patients battling locally advanced breast cancer.
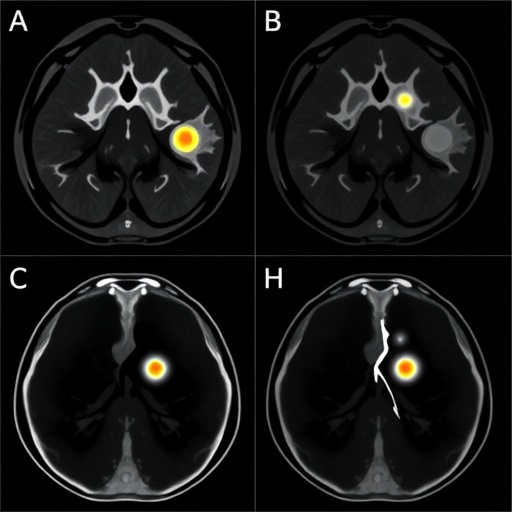
The role of imaging biomarkers in oncology has rapidly evolved, with functional imaging techniques such as PET/CT providing unparalleled insight into tumor metabolism and proliferation. [18F]FLT, a radiotracer used to assess cellular proliferation by tagging thymidine analog uptake, emerges as a promising candidate in this domain. By measuring TBR—the quotient of tumor SUV relative to the background parenchymal tissue—clinicians aspire to refine therapeutic decision-making with precision beyond conventional tumor size assessment.
Central to this study was the analysis of 90 breast cancer patients across 17 centers, each undergoing a regimented imaging protocol that involved three [18F]FLT PET/CT scans at distinct treatment stages: pre-treatment baseline, post-first NAC cycle, and post-chemotherapy completion. This temporal approach enabled researchers to meticulously track dynamic changes in tumor metabolism alongside volumetric adjustments, juxtaposing functional and anatomical parameters.
.adsslot_gfvHbKxGRz{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_gfvHbKxGRz{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_gfvHbKxGRz{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Surprisingly, when considered independently, classical metrics such as tumor size and TBR values—both mean and maximum uptake ratios—demonstrated limited sensitivity and specificity in foretelling pathological response. The highest area under curve (AUC) statistic achieved for these metrics individually hovered at a modest 0.682, signaling suboptimal predictive capacity and underscoring the complexity of tumor biology and response heterogeneity.
Delving deeper, the investigators innovatively combined PET-derived functional data with CT-based anatomical measurements, thereby forming an integrated diagnostic model. This hybrid approach significantly amplified prognostic accuracy, with the combined model yielding AUC scores of 0.731 and 0.833 for baseline and post-chemotherapy scans respectively. Notably, evaluating the percentage change between these scans realized an even more striking AUC of 0.875, heralding a new benchmark for predictive modeling in this context.
Intriguingly, mid-NAC imaging, a time point often presumed to be critically informative, did not showcase substantial diagnostic value in either standalone or combined models. The peak AUC at this interim stage was a mere 0.626, raising pivotal questions regarding optimal imaging windows and the biological underpinnings manifesting during chemotherapy.
These findings collectively illuminate the complementary nature of functional and structural imaging parameters in capturing the multifaceted response of tumors to systemic treatment. The nuclear medicine community has long speculated on the merit of combining metabolic indicators with anatomical changes, and this study offers compelling empirical support for this paradigm. Importantly, the tumor to background parenchymal ratio serves as a nuanced functional biomarker, reflecting proliferative activity relative to surrounding healthy tissue rather than absolute uptake values alone.
Further, the large multicenter design lends robust external validity to the results, suggesting their generalizability across diverse clinical environments. Harnessing prospective data, though analyzed retrospectively here, reduces the bias often inherent in smaller, single-institution studies. This bodes well for potential clinical translation, where standardized imaging protocols can be implemented to guide therapeutic personalization.
Enhanced predictive accuracy in NAC response assessment carries profound implications. For patients, it could mean earlier, more informed decisions to modify or escalate treatment regimens, avoiding ineffective chemotherapy cycles and attendant toxicities. For clinicians, these insights empower a more data-driven approach to patient management, balancing efficacy with quality of life considerations.
However, challenges persist in integrating advanced imaging biomarkers into routine clinical workflows. Factors such as cost, accessibility, and expertise in interpreting dynamic PET/CT metrics must be addressed to realize widespread adoption. Additionally, further prospective trials are warranted to validate these findings and explore their utility in conjunction with emerging molecular and genomic biomarkers.
Beyond breast cancer, the methodological principles elucidated here—leveraging TBR in a combined functional-anatomical model—may extend to other malignancies where neoadjuvant chemotherapy plays a pivotal role. The study’s innovative use of serial imaging time points offers a template for dynamic treatment monitoring adaptable to diverse oncologic contexts.
Moreover, the study contributes critical knowledge to the evolving field of personalized oncology. By delineating how complex tumor-host interactions manifest on advanced imaging, clinicians gain a window into the temporal biological landscape of treatment response, paving the way for adaptive precision medicine strategies.
In summation, this comprehensive study underscores the transformative potential of integrating tumor size with [18F]FLT PET/CT derived tumor to background parenchymal ratios to predict neoadjuvant chemotherapy efficacy in breast cancer accurately. Its findings set the stage for future research priorities and clinical applications aiming to optimize patient outcomes via sophisticated imaging biomarkers.
As the oncology community continues to harness technological advancements, studies like these exemplify the vital intersection of molecular imaging and therapeutic innovation. They bring hope for a future where cancer treatments are tailored with unprecedented accuracy, sparing patients unnecessary interventions and enhancing survival prospects.
The promising results here resonate with the broader quest for biomarkers that are not only precise and reproducible but also practical and minimally invasive. The integration of functional metrics with conventional imaging might well represent the next leap forward in oncological diagnostics and patient care management.
Ultimately, this impactful research conducted across multiple leading centers enriches the scientific dialogue surrounding breast cancer treatment and shines a spotlight on the indispensable role of multimodal imaging in contemporary oncology.
Subject of Research: The predictive value of tumor to background parenchymal ratio (TBR) in [18F]FLT PET/CT imaging for assessing breast cancer response to neoadjuvant chemotherapy.
Article Title: Exploring the role of tumor to background parenchymal ratio of the [18F]FLT PET/CT measures in determining response to neoadjuvant chemotherapy in breast cancer: a multicenter study.
Article References:
Mohebbi, A., Asli, F., Mohammadzadeh, S. et al. Exploring the role of tumor to background parenchymal ratio of the [18F]FLT PET/CT measures in determining response to neoadjuvant chemotherapy in breast cancer: a multicenter study. BMC Cancer 25, 1139 (2025). https://doi.org/10.1186/s12885-025-14534-w
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14534-w
Tags: [18F]FLT PET/CT imagingbreast cancer treatment strategieschemotherapy response predictionfunctional imaging techniquesimaging biomarkers in oncologymulticenter breast cancer studyneoadjuvant chemotherapy imagingpersonalized cancer therapy decisionsstandardized uptake values analysistumor growth monitoringtumor metabolism assessmenttumor-to-parenchyma PET ratio